Each year, around 60 000 people in the UK experience an out-of-hospital cardiac arrest (Fisher, 2020). Despite improvements in cardiopulmonary resuscitation and the use of evidence-based interventions, the average survival to hospital discharge for cardiac arrest out of hospital in England is 8.6% (Resuscitation Council, 2015).
The introduction of additional diagnostic tools, such as focused cardiac ultrasound (FoCUS), aid treatment and management of patients at the point of care (Andrus and Dean, 2013). FoCUS is an investigative tool that examines cardiac function with a portable device at the point of care (Andrus and Dean, 2013). The Resuscitation Council published guidance in 2021 on the use and importance of FoCUS in cardiac arrest management by trained clinicians (Soar et al, 2021a).
Multiple terms are used when speaking about ultrasound, for example echocardiography, sonography and point-of-care ultrasound as well as FoCUS. These all relate to the use of a probe to examine the heart and its structures through sound waves to create an image of the internal structures. Although mainly used to detect traumatic injury, ultrasound can also be used to assess myocardial contractility in cardiac arrests (Andrus and Dean, 2013; Blanco and Martínez Buendía, 2017).
Ultrasound for cardiac arrest patients is widely available in hospitals; it is becoming more prevalent in the prehospital setting, although there are acknowledged concerns regarding the quality of evidence supporting its use (Huis in ‘t Veld et al, 2017; Brown and Quinn, 2021).
FoCUS has been found to have a role in the identification of potential reversible causes of cardiac arrests, such as hypovolaemia and hypoxia (Kedan et al, 2020). Although FoCUS is frequently implemented to guide resuscitation, questions surround its prognostic value and ability to affect patient survival (Blaivas and Fox, 2008).
It is important to review the literature surrounding this topic to examine the role of FoCUS, its impact on survival rates and how it can guide further research and practice. This review of the literature will examine the impact FoCUS has on patient management and treatment, and evaluate its role in prehospital cardiac arrests and whether it is a valuable tool prehospitally.
Method
A systematic literature search was undertaken between 22 February and 1 March 2021. Two databases, PubMed and ScienceDirect, were searched using keywords relating to the review and combined using Boolean operators and search parameters. These databases were chosen based on their ability to produce scientific and medical research. PubMed provides biomedical and scientific literature through a database (Ossom Williamson and Minter, 2019). ScienceDirect provides scientific and medical literature (Elsevier, 2021). However, it includes only Elsevier papers, which is a limitation of the literature search.
For this rapid review, only two databases were chosen as this was believed to be sufficient to cover the large volume of relevant papers. It was acknowledged during the search that these two databases would not cover all potential papers. PubMed was chosen because of its to its scientific background and, alongside this, ScienceDirect was chosen as a second database to strengthen the search. There were more hits from ScienceDirect than PubMed.
A PICO (patient/population, intervention, comparison and outcomes) structure was used to identify key terms such as ‘cardiac arrest’, ‘ultrasound’, ‘cardiac activity’, and ‘return of spontaneous circulation’. The following synonyms and related words were extrapolated from the main terms and included in the search strings: ‘cardiopulmonary resuscitation’, ‘life support’, ‘echocardio*’, ‘focused cardiac ultrasound’, ‘FoCUS’, ‘point of care ultrasound’, ‘sonograph*’, ‘cardiac’, ‘motion’, ‘activity’, ‘contractility’, ‘standstill’, ‘outcome’ and ‘ROSC’.
A search log was used to record each literature search, with results limited to papers published from 2004 onwards, in English and with the full text available. Inclusion criteria were determined to be adult participants, where patient outcomes and cardiac activity were measured with the use of ultrasound.
Literature relevant to the use of ultrasound in medical cardiac arrests where the prevailing cardiac rhythm was non-shockable was primarily sought to address the review question. Records were initially screened by title and abstract, and excluded systematic reviews, animal studies and literature focusing on traumatic cardiac arrests, where cardiac arrest was not the focus of the ultrasound study and where transoesophageal echocardiography was used. Finally, the literature was critiqued for rigour using the Hek and Moule (2006) critiquing framework during the full text screening phase.
Results
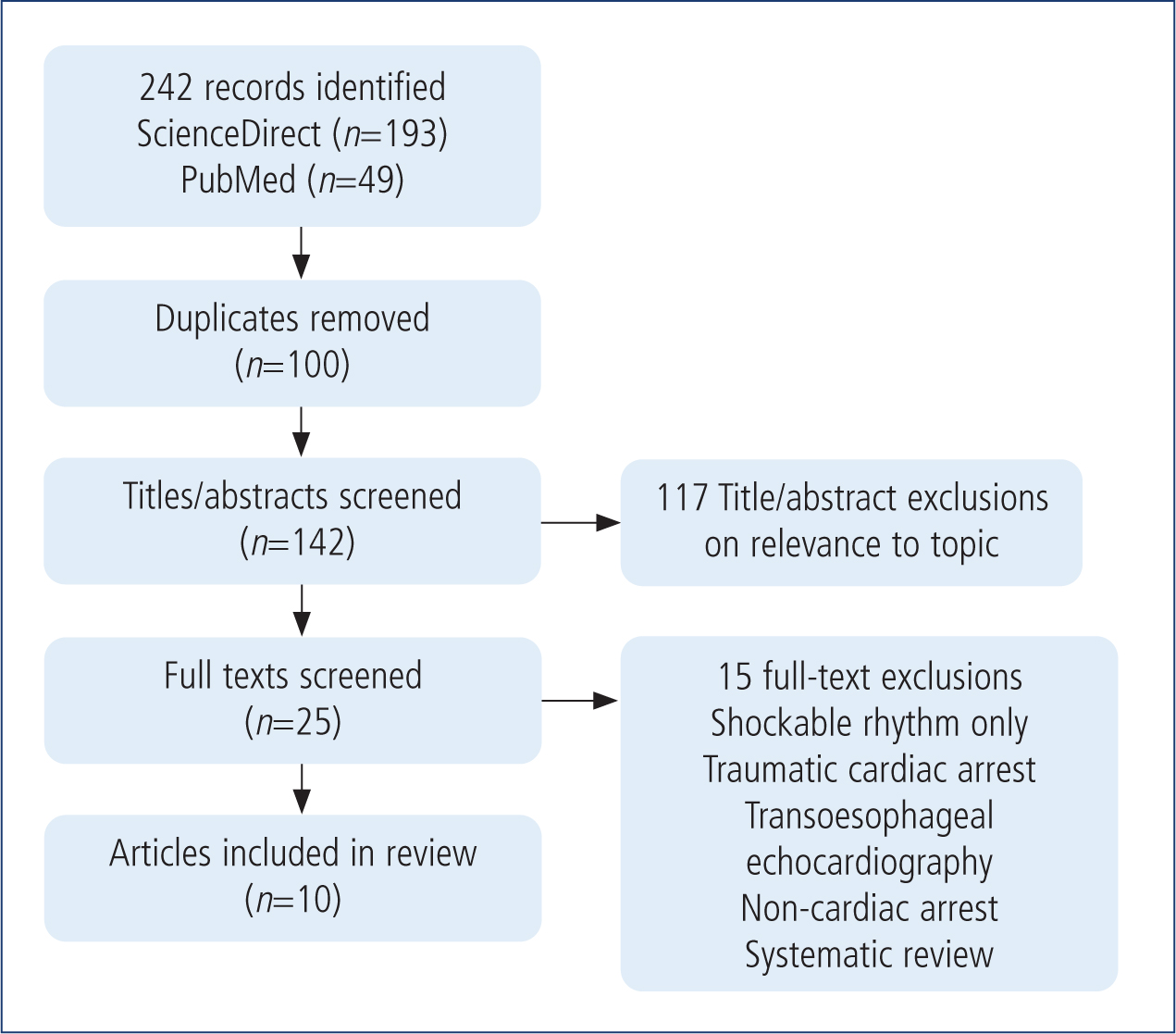
Initially, 242 records were identified through all the searches, with 193 from ScienceDirect and 49 from PubMed. One hundred duplicates were removed based on database overlap. Of the 142 titles/abstracts screened, 117 were excluded because of a lack of relevance and for not meeting the inclusion criteria. Final screening and critique were performed on 25 full text articles and 15 were removed based on the exclusion criteria not being met. A total of 10 articles were included (Figure 1) (summarised in Table 1).
| Author, year, title | Methods | Results | Conclusion |
|---|---|---|---|
|
Salen et al (2005)
|
Aim: evaluate the ability of cardiac sonography performed by emergency physicians to predict resuscitation outcomes of cardiac arrest patients |
23 (68%) patients with PEA had no cardiac motion identified compared to 11 (32%) with cardiac activity. Eight patients with pseudo PEA achieved a ROSC with one surviving to hospital discharge. Of the 23 patients in PEA with no cardiac activity, none gained a ROSC. The accuracy of FoCUS to predict survival to hospital discharge versus death was 0.87% (95% CI). | The data supports the idea that cardiac sonography can provide information that may help in making pertinent management decisions regarding CPR |
|
Breitkreutz et al (2010)
|
Aim: evaluate the feasibility of focused echocardiography in prehospital resuscitation and the influence on patient management |
51% of patients undergoing CPR were in PEA, of whom 75% had cardiac activity. In the remaining 13 (25%) patients, there was no cardiac motion. Thirty-seven patients were found to be in asystole; 13 of these had cardiac motion and 24 did not. 55% of patients in PEA with cardiac motion survived to admission, compared with 8% who did not have cardiac motion. | FoCUS has the ability to diagnose potential reversible causes and alter management. However further research into its effect on patient outcomes is warranted. |
|
Aichinger et al (2012)
|
Aim: evaluate the ability of emergency echocardiography (EE) to predict outcomes in cardiac arrest patients |
Out of the 42 study patients, 11.9% survived to hospital admission; 23.8% of patients had cardiac activity on initial EE. Of the 32 people who had no cardiac movement on the initial EE, one (3.1%) survived to hospital admission. Four out of the 10 patients with cardiac movement on the EE survived to hospital admission (P=0.008). Cardiac standstill on EE had a PPV of 96.6% for death. | The results support the idea that focused echocardiography is an additional tool for evaluation of outcome in patients. However, larger studies are needed to find out if it can be used to predict outcome. |
|
Chardoli et al (2012)
|
Aim: examine the utility of echocardiography in detecting reversible causes and predicting the resuscitation outcomes |
50 patients were found to be in PEA, of those 78% had cardiac activity and 22% without. Of those with cardiac activity 17 (43%) gained a ROSC. Compared to zero in the absence of cardiac activity. | It can accurately detect some reversible causes however, fails to represent a significant impact on the outcome of patients resuscitations. Identifying ventricular activity assists in predicating the probability of ROSC. |
|
Cebicci et al (2014)
|
Aim: examine the benefit of cardiac sonography for predicting survival. |
A total of 75 patients (18.3%) were in PEA compared to 290 (70.7%) in asystole. 46 (61.3%) patients in PEA gained a ROSC compared to 9 (3.1%) in the asystole group. Of those in PEA who gained a ROSC, 45 (60%) survived to 24 hours. | Ultrasound is effective in detecting cardiac activity and estimating subsequent survival. It is an effective diagnostic tool for the cause of asystole and PEA. There is strong association between cardiac activity and ROSC. |
|
Flato et al (2015)
|
Aim: evaluate the feasibility of echocardiography in non-shockable cardiac arrest patients in an intensive care unit (ICU) and its relation to patient outcomes |
17 (34.7%) patients were found to be in asystole and 32 (65.3%) in PEA. 27 (55.1%) of the PEA patients had cardiac motility and five (10.2%) had none. 19 patients with pseudo PEA sustained a ROSC, with six surviving to hospital discharge. One patient with true PEA sustained a ROSC with none surviving to hospital discharge. | Echocardiography performed during a cardiac arrest allows for reliable image acquisition. It identifies a subgroup of patients who may benefit from continued resuscitation efforts. |
|
Gaspari et al (2016)
|
Aim: determine whether cardiac activity on ultrasound during advanced cardiac life support is associated with improved survival |
263 patients had cardiac activity. 134 (51.0%) gained a ROSC, 76 (28.9%) survived to hospital admission and 10 (3.8%) survived to discharge. In the 530 patients with no cardiac activity, 76 gained a ROSC, 38 survived to admission and three to discharge. Patients in asystole had a PPV for ROSC, and survival to hospital admission and survival to discharge of 0.90, 0.94 and 0.99 respectively. Those with PEA had a PPV for ROSC, survival to hospital admission and survival to discharge of 0.79, 0.91, 1.00 respectively. | Point-of-care ultrasound identified patients with higher likelihood of survival as well as those who would benefit from interventions outside the strict ACLS protocol. Ultrasound may also identify patients where prolonged resuscitation may not provide measurable benefit. |
|
Kim et al (2016)
|
Aim: evaluate the correlation between echocardiography findings and ROSC in patients with an out-of-hospital cardiac arrest (OHCA) and to examine whether echocardiographic cardiac standstill duration can be used to predict ROSC. |
39 patients presented with asystole. 21 had a ROSC and 18 died. Eight patients presented in PEA with six gaining a ROSC. One patient with PEA had no cardiac motion and did not achieve a ROSC. The other seven patients in PEA had cardiac motion with patients gaining a ROSC. Sensitivity of cardiac standstill for predicting non ROSC was 100.0%, specificity was 17.9% and PPV was 46.5%. | No patients found in cardiac standstill gained a ROSC. However, further research is needed into the association of cardiac standstill and ROSC. |
|
Ozen et al (2016)
|
Aim: investigate the hypothesis that in patients with detectable ventricular wall motion (VWM) in cardiac ultrasonography during CPR, survival rate is significantly more than in patients without VWM. |
In patients with VWM, ROSC was obtained in 72.8% (n=56: p<0.001). In patients without VWM, ROSC was obtained in 5.8%(n=3). No patients without VWM survived at the end of 1 month whereas eight patients with VWM survived to 1 month. | The absence of VWM is highly correlated with the demise of those patients and early termination of CPR efforts may be considered. Further randomised controlled trials are needed to have higher level of evidence. |
|
Reed et al (2017)
|
Aim: can prehospital paramedic responders perform satisfactory prehospital echo in life support (ELS) during the 10s pulse check window and does prehospital ELS adversely affect the delivery of cardiac arrest care? |
40 patients were included in analysis with 20 in asystole and five in PEA. A total of 16 (41%) patients achieved ROSC and six survived to hospital admission. In 42% of patients, no cardiac movement was identified. | ELS is more likely to be performed in patients for whom a decision to discontinue resuscitation efforts is being considered. Further studies will be needed to demonstrate improved outcomes from identifying patients for whom further resuscitation and transportation is futile |
ACLS: advanced cardiac life support; CPR: cardiopulmonary resuscitation; PEA: pulseless electrical activity; PPV: positive predictive value; ROSC: return of spontaneous circulation
Discussion
FoCUS provides real-time anatomical and physiological data that can be used to assess a patient's condition. The 2021 Resuscitation Council guidelines for adult advanced life support state that FoCUS must not be used as the sole indicator for terminating resuscitation or interrupting chest compressions (Soar et al, 2021a; 2021b).
In non-shockable cardiac arrest rhythms, there are significant challenges in identifying the cause, so the use of ultrasound has the potential to improve the management of these patients (Hussein et al, 2019).
It was acknowledged during the examination of the literature that different papers used a variety of terminology when explaining the use of ultrasound; these are used within this rapid review for authenticity.
Key themes identified within the literature were prognostication, identification of reversible causes, and true pulseless electrical activity (PEA) versus pseudo PEA.
Prognostication
It is clear there is the need for an accurate tool to determine which patients may have an better chance of surviving a cardiac arrest. The assessment of cardiac activity by FoCUS provides prognostic value of the patient's condition to facilitate improved resuscitation outcomes (Breitkreutz et al, 2010; Aichinger et al, 2012; Chardoli et al, 2012).
Aichinger et al (2012) examined cardiac activity identified with FoCUS and found that only one patient with cardiac standstill survived to hospital admission, compared to four who had cardiac motion on initial FoCUS, so patients with cardiac motion had an better chance of survival and may benefit from further intervention.
Furthermore, Aichinger et al (2012) found cardiac standstill had a positive predictive value (PPV) for death in patients without cardiac activity of 96.6%, evidencing the prognostic value of FoCUS on predicting outcomes (Aichinger et al, 2012).
Two studies concluded that the absence of cardiac motion was associated with lower rates of return of spontaneous circulation (ROSC) (Aichinger et al, 2012; Ozen et al, 2016). In addition, Cebicci et al (2014), Kim et al (2016) and Reed et al (2017) all found cardiac standstill with FoCUS to be a predictor of resuscitation failure, suggesting these patients may not benefit from further interventions and FoCUS may have the ability to support decisions when terminating resuscitation.
In comparison, the prognostic value of cardiac activity may mean it is an accurate predictor of survival (Gaspari et al, 2016).
Gaspari et al (2016) conducted a large multicentre study of 793 patients where FoCUS was used in cardiac arrest. They concluded that cardiac activity on FoCUS was associated with higher rates of ROSC as evidenced also by Aichinger et al (2012)(Gaspari et al, 2016). However, three patients with no cardiac activity survived to hospital discharge, despite the higher association between cardiac activity and the likelihood of achieving ROSC (Gaspari et al, 2016). Undoubtedly, those with cardiac activity may have a better outcome because of prolonged resuscitation efforts, although it is thought this is not the primary cause of increased survival rates, with little association between these variables (Gaspari et al, 2016). Although this study had a large sample size, there was no randomisation or blinding, which increased the risk of bias.
Moreover, Gaspari et al (2016) and Ozen et al (2016) both measured survival to hospital admission and discharge alongside ROSC, while Cebicci et al (2014) focused on whether cardiac activity was a reliable predictor for 24-hour survival. However, none of these reported on the long-term outcomes of the patients being studied. Despite the growing body of evidence surrounding the association between cardiac activity and increased likelihood of ROSC, it is important to note a small number of patients survive even when cardiac standstill is identified through ultrasound (Gaspari et al, 2016; Ozen et al, 2016). As a result, termination of resuscitation should not be decided from FoCUS alone, as the current Resuscitation Council guidelines state, but used as an additional tool to guide decisions (Soar et al, 2021a; 2021b).
It is evident that patients with cardiac activity have a higher likelihood of gaining ROSC than those with cardiac standstill. Potentially, the prognostic value FoCUS provides could be harnessed in identifying those who may benefit from further interventions.
Identification of reversible causes
The European Resuscitation Council Guidelines 2021 state that reversible causes of a cardiac arrest should be ruled out and treated. These are hypoxia, hypo/hyperkalaemia, hypothermia, hypovolaemia, tension pneumothorax, tamponade, thrombus and toxins (Soar et al, 2021a; 2021b). Early identification and treatment affect patient management and increase the chances of survival (Breitkreutz et al, 2010; Hussein et al, 2019).
Breitkreutz et al (2010) identified 33 patients with cardiac activity and reduced left ventricle function, pericardial tamponade, a dilated right ventricle or hypovolaemia. ROSC was gained after pericardiocentesis in the five patients with pericardial tamponade (Breitkreutz et al, 2010).
Similarly, Gaspari et al (2016) identified 34 patients with pericardial effusion and 13 were subsequently treated with pericardiocentesis (Gaspari et al, 2016).
Using FoCUS to identify reversible causes of a cardiac arrest enables clinicians to provide the correct intervention, improving the chances of survival, as demonstrated in the findings of Breitkreutz et al (2010).
In contrast, Chardoli et al (2012) examined the use of FoCUS in detecting reversible causes in PEA cardiac arrests compared to resuscitation without FoCUS and found no significant difference in the survival outcomes of either group (P=0.52), in contrast to the conclusions of Breitkreutz et al (2010) and Gaspari et al (2016).
Therefore, despite results showing higher ROSC rates with the use of FoCUS, when compared to FoCUS not being used, there is little difference in outcome, questioning the true benefit. However, it is important to note that Chardoli et al (2012) concluded that FoCUS can reliably detect reversible causes, subsequently improving chances of survival, although larger sample sizes are needed to fully support their conclusions.
Breitkreutz et al (2010) concluded that the use of FoCUS resulted in changes to medical therapy or destination in a large number of patients. This shows that using FoCUS to visualise the heart and its structures can provide clinicians with a reliable assessment of the patient's condition, identifying those who need further treatment for a better chance of survival (Breitkreutz et al, 2010).
Similarly, Gaspari et al (2016) conducted the first study that proved ultrasound identified reversible causes and increased survival rates, with 15.4% of patients surviving to hospital discharge who were found to have a cardiac tamponade compared to 1.3% who had no reversible causes identified with FoCUS. Although they concluded that the presence of cardiac activity was mostly associated with high ROSC rates, they supported the inclusion of ultrasound into the advanced cardiac life support protocol (Gaspari et al, 2016).
Despite the findings of Breitkreutz et al (2010), their focus was on the feasibility of the use of FoCUS prehospitally, while the primary outcome of Gaspari et al's (2016) study was survival to hospital admission.
Although Gaspari et al's study (2016) demonstrates a higher survival rate in patients who had reversible causes identified compared to all other patients in their study, there is a high risk of bias because of a lack of blinding of the results, which was also seen within the research by Breitkreutz et al (2010). Despite low sample sizes—a common limitation seen throughout these studies—FoCUS is evidently altering patient treatment through its diagnostic value.
True PEA versus pseudo PEA
True PEA is defined as electrical activity presented on a cardiac monitor without cardiac motion on ultrasound (Salen et al, 2005). Pseudo PEA or a low-flow state is the presence of some cardiac motion with electrical activity (Salen et al, 2005).
Chardoli et al (2012) studied resuscitation outcomes for PEA arrest patients based on findings from cardiac ultrasound. The presence of pseudo PEA had a PPV of 43% for ROSC compared to a PPV of 100% for death in the true PEA group (Chardoli et al, 2012). This suggests that patients who present with pseudo PEA are more likely to achieve ROSC than those in true PEA. This may be because the knowledge of cardiac activity influences treatment decisions, such as prolonging or ceasing resuscitation efforts, that affect ROSC outcomes.
Chardoli et al (2012) identified more patients in pseudo PEA than Salen et al (2004), who also found greater ROSC rates in the pseudo PEA group than those with true PEA, indicating that the presence of pseudo PEA has an increased chance of a patient achieving ROSC.
This is consistent with other literature reviews published regarding the 100% PPV for death in true PEA (Blyth et al, 2012; Chardoli et al 2012; Hussein et al, 2019). Salen et al (2005) had a lower sample size (70) than Chardoli et al (2012) (100), which affects the reliability of the results. Moreover, Salen et al (2005) and Chardoli et al (2012) used convenience sampling, increasing the risk of bias (Crowther and Lancaster, 2012).
In contrast, Breitkreutz et al (2010) found 10% of patients with no cardiac motion survived, recording one of the highest survival rates in patients with no cardiac activity. Although this is a statistic of note, it is of low significance when examining the full range of data because of other variables contributing to increased survival rates.
When comparing the findings from Salen et al (2005) and Flato et al (2015), both noted similar results with pseudo PEA having an increased predictive value for ROSC compared to a high predictive value for non ROSC in those presenting with true PEA. This shows the increasing association between pseudo PEA and increased ROSC rates, because, if it is identified, alternative management can be provided. If pseudo PEA can be identified, patients with this condition are more likely to survive, as the evidence demonstrates.
Therefore, identifying these patients allows for more focused treatment and management that patients may not have received if pseudo PEA had not being diagnosed by FoCUS because FoCUS was not available.
Conclusion
The evidence shows there is an association between cardiac activity identified with FoCUS and an increase in ROSC rates. Moreover, these studies support the poor prognostic value of identifying cardiac standstill on FoCUS. The use of FoCUS for improving survival is not statistically significant; however, there is a higher likelihood of survival because it can aid decision making. There is little evidence surrounding paramedic or prehospital use; the need for high-quality evidence on prehospital use of FoCUS is paramount.
Patients in whom cardiac activity was identified using FoCUS were more likely to achieve ROSC than those without such activity; however, it remains that those with cardiac standstill identified with FoCUS had a higher PPV for death.
In addition, the identification of reversible causes using FoCUS had a positive impact on ROSC rates because it meant practitioners could provide early intervention, increasing the likelihood of the patient gaining ROSC.
Moreover, the identification of cardiac activity with FoCUS was associated with an increase in ROSC potentially because of its ability to alter patient treatment.
Furthermore, the use of FoCUS to distinguish between true and pseudo PEA has shown to aid decision making as the presence of pseudo PEA increases the likelihood of ROSC. Although the data suggest the presence of cardiac activity is highly associated with ROSC, there is little literature surrounding long-term outcomes of patients, affecting the ability of FoCUS to determine survival.
FoCUS is an effective tool in identifying cardiac activity in non-shockable rhythms, potentially aiding treatment decisions, including additional interventions or as an additional tool when deciding whether to terminate a resuscitation.
Recommendations
It is evident that FoCUS has a role in the treatment and management of cardiac arrest. However, to inform and adapt policies, there needs to be stronger research evidence into its use with larger sample sizes.
FoCUS is currently performed only by specialist trained clinicians, such as advanced paramedics and doctors, in the prehospital setting. It has been shown to benefit patient outcomes and, if implemented in prehospital care, it could potentially be carried out by paramedics who have received training.
However, it may not be feasible to implement FoCUS on a standard ambulance when weighing up the current evidence in relation to prevalence and impact against the potential cost and training required.
Therefore, if the use of FoCUD is to be advanced, paramedics who work on rapid response units primarily tasked to care for patients in life-threatening circumstances, including those in cardiac arrest, would benefit from training on the use of FoCUS and it being implemented into their skillset.
The most recent resuscitation guidelines advocate for the use of FoCUS, although it should be used only as a tool in conjunction with other parameters when deciding termination of resuscitation because of a lack of high-quality evidence (Soar et al, 2021a; 2021b).
Experimental studies to compare the outcomes of those who receive FoCUS and those who do not are needed.
Overall, FoCUS could change policy and practice with effective education and more research supporting its diagnostic ability to improve survival rates in non-shockable cardiac arrests, both prehospitally and in hospital.
