Interactive virtual reality (VR) models that allow the user to inspect and manipulate computer-generated real or fabricated three-dimensional (3D) sensory environments in real-time are becoming widely used in health professions teaching (Roth et al, 2015; de Boer et al, 2017). Sometimes VR and simulation are used interchangeably; the authors consider a VR learning experience to include the following characteristics:
VR experiences can be delivered to participants in a variety of ways, including computer or mobile device screens, and in VR rooms using head-mounted displays (McGaghie et al, 2010), which is the basis of the present study.
In health profession education, a small number of studies report the use of VR and it is predominantly used for educational motor skills training such as surgery, clinical testing of protocols and undergraduate medical anatomical training (Pensieri and Pennacchini, 2014; Kockro et al, 2015; Kim et al, 2017; Joda et al, 2019). However, the authors are not aware of any studies describing its use in teaching paramedical anatomy and physiology.
It has been suggested that virtual 3D models improve knowledge of subject matter by helping learners integrate knowledge with practical application (Trelease and Nieder, 2013; de Boer et al, 2016). It potentially complements didactic teaching methods, although studies such as Courtier et al (2016) report uncertainty of educators and students regarding whether digital resources make the best use of limited time (Courtier et al, 2016). VR teaching methods have been compared with traditional didactic lectures and other digital teaching methods (Kyaw et al, 2019); however, whether they are suitable to include in problem-based learning (PBL)-style classes remains unexplored.
There is ongoing debate about the effectiveness of VR in terms of improving knowledge and skills, and acquiring attitudes (Tam, 2010). A recent meta-analysis of eight studies using VR for health professions education found that it slightly improved knowledge acquisition when compared with comparator education methods (standardised mean difference [SMD]=0.44; 95% CI 0.18-0.69; n=603 participants) and four studies found that VR improves health professionals’ cognitive skills when compared with traditional learning (SMD=1.12; 95% CI 0.81-1.43; n=235) (Kyaw et al, 2019). It has been demonstrated in several studies that surgical simulation training improves individual performance and reduces error rate (McGaghie et al, 2010). In cardiovascular fellows, it has also been demonstrated to improve angiography skills and knowledge (Westerdahl and Henry, 2016). A Cochrane review of eight trials found that it improved the operative laparoscopic performance of surgical trainees (Nagendran et al, 2013).
In anatomy teaching, a study has reported improved knowledge in a randomised, controlled trial, having developed a computer-generated three-dimensional anatomical ear model (Nicholson et al, 2006), while another study found no association between students’ spatial ability and laryngeal anatomy learning (Tan et al, 2012). Guimarães et al (2019) reported that computer-assisted learning in cardiovascular and musculoskeletal anatomy has a positive dose-dependent effect on spatial abilities in medical students, although this uses a 2D rather than 3D environment.
The findings for learners’ attitudes and satisfaction with VR were mixed (Kyaw et al, 2019). Several published studies report satisfaction in the student population, in the absence of a control group (Keedy et al, 2011; Tan et al, 2012; Kockro et al, 2015). None of the studies reported any patient-related outcomes, behaviour change, or unintended or adverse effects of VR. Furthermore, the impacts of VR on users from a physiological and cognitive perspective, as well as in behavioural and social dynamics, have been hypothesised as potential barriers to use, although this has not yet been studied (Kenwright, 2018).
The authors developed a prototype of a virtual, immersive, and interactive cardiac anatomy tutorial for paramedical cardiovascular anatomical and physiology training. Although the use of computer? generated 3D anatomical models has potential advantages over traditional anatomy and physiology instruction methods, the time and financial resources needed to develop and adopt these models are significant. The aim of the study is to demonstrate a VR-based exercise integrated into a PBL tutorial to teach cardiac anatomy in a cohort of undergraduate paramedics and assess its impact on knowledge and student satisfaction.
Methods
Setting
The study was performed with first-year undergraduate paramedical students at the University of Limerick (UL) beginning in October 2018. The anatomy and physiology module covers nine organ systems whose learning objectives are defined by the undergraduate paramedic curriculum, including cardiovascular, respiratory, reproductive, core chemistry, skeletal, renal, central nervous system, endocrine and gastro/digestive systems. The curriculum is delivered over 12 weeks with an exam at the end of each week.
Each exam consists of 25 single best answer questions on that week's anatomy. The question set is selected from the UL paramedical studies question bank. The single best answer question bank was developed for the anatomy course by a panel of experienced paramedic educators. Students are required to read the multiple choice question text and select the correct response option from the list provided. A maximum of 1 minute was allowed to answer each item. Optical marking sheets were used to record response data, which were processed using MultiQuest software, version 2.92 (Speedwell Software Ltd, Cambridge UK).
Educational delivery and attendance
The anatomy modules are delivered through PBL tutorials with text materials and a 2-hour compulsory lecture each week. Anatomy for the cardiovascular unit was taught using VR-based exercises incorporated into existing compulsory PBL pedagogy. Attendance at all sessions is mandatory.
For the VR class, head-mounted displays are placed over the user's head which show the user projected 3D images of the VR room used for learning. The VR room is a projector-based immersive 3D experience which, in our case, displays a 3D cardiovascular system (CVS). It can involve multiple users at the same time and combines multiple senses (audio, visual, touch, and movement), each of which influences the immersive experience. Students who did not access the equipment during the tutorial had access to the VR equipment the following week. Figure 1 shows the VR system and its uses.

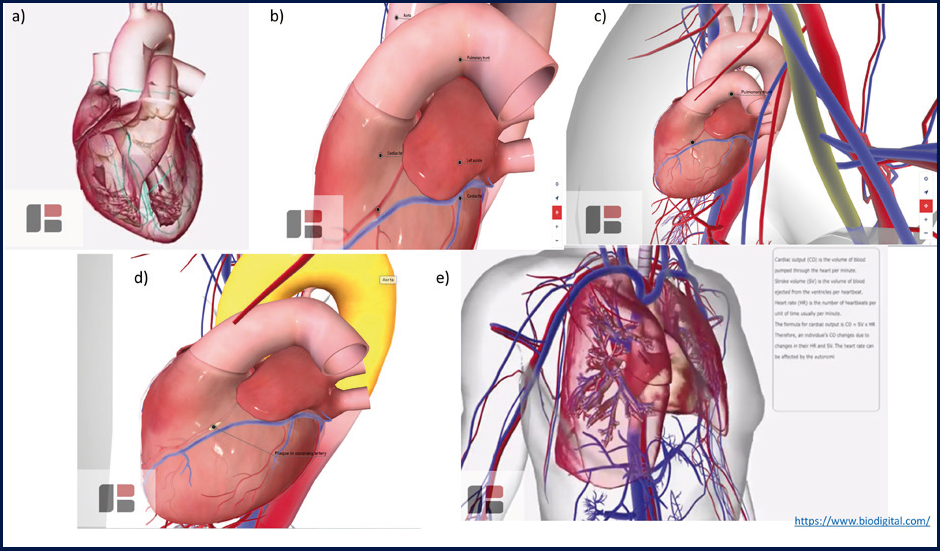
Materials: 3D cardiovascular training lesson design
A VR 3D anatomical model of the CVS was designed and piloted over 8 weeks (Figure 2). The basics of the CVS was written into a script that satisfied the Pre-Hospital Emergency Care Council and National Qualification in Emergency Medical Technology guidelines. This was done using textbooks as the main source, to ensure accuracy of the information. The level of detail was basic/moderate but overall it was adequate. Over an 8-week period, a video consisting of everything discussed in the CVS script was made using virtual reality. The programmes used were 3D Organon®, Sharecare VR® and Biodigital®, although not all of them featured in the final video. Screenshots of the VR experience show how once the user has touched the model, the system will colour the associated anatomical structure and will provide a text note/voiceover with the information (Figure 2). The user can switch between details of motor, sensory or other functions associated to the touch areas.
Study participants and design
This was a cohort study. All first-year students in the paramedic course at UL from 2018 to 2019 were eligible to take part in the study. The subjects were recruited in October 2018.
Data collection
The exam used in this study followed the structure familiar to the students in questioning format, testing time, and administration, used throughout the module.
The overall module score was calculated as a combination of the student's marks across all 12 weeks, excluding the cardiovascular exam. The goal of the anatomy and physiology module is that the students reach a minimum standard of knowledge to be applied during paramedic practice skills training. Upon completion of the anatomy and physiology module, students should be able to outline the structure and function of the body. The module score represents their knowledge of the respiratory, musculoskeletal, digestive, endocrine, blood, skin, nervous, urinary, reproductive systems and the senses, which are examined across eight multiple choice question exams in the same format as the cardiovascular exam.
A survey to understand students’ experiences of having completed the cardiovascular module of their training as part of a hybrid PBL curriculum was distributed in November 2018 to all first-year paramedic students (n=19). Contact details were sourced from a school administrator and all graduates were forwarded an invitation to take part in this study by an independent gatekeeper. All participants were made aware of the voluntary nature of the survey with no identifying information collected. The response rate was 79% (n=15).
Ethical approval
This study was approved by the Education and Health Science Faculty Ethics Committee (2018_09_10_EHS). Written informed consent was obtained from all individual participants included in the study by a study team member independent from the paramedics course.
Statistical analysis
The Shapiro-Wilk normality test was carried out on the scores of the cardiac unit exam and overall physiology and anatomy module. The p-value (p=0.734) was found to be greater than 0.05, implying that the distribution of the exam results is assumed to be normal. The difference in participants' mean score on the cardiac exam and overall module exam was tested using a one-sided paired t-test. p-values less than 0.05 were considered statistically significant. Quantitative data were analysed using the R Statistical Package. A descriptive analysis of quantitative data was completed to describe their experience of VR-based anatomy learning. Variables that are known to influence the learning experience were descriptively summarised among the subjects.
Results
Educational performance
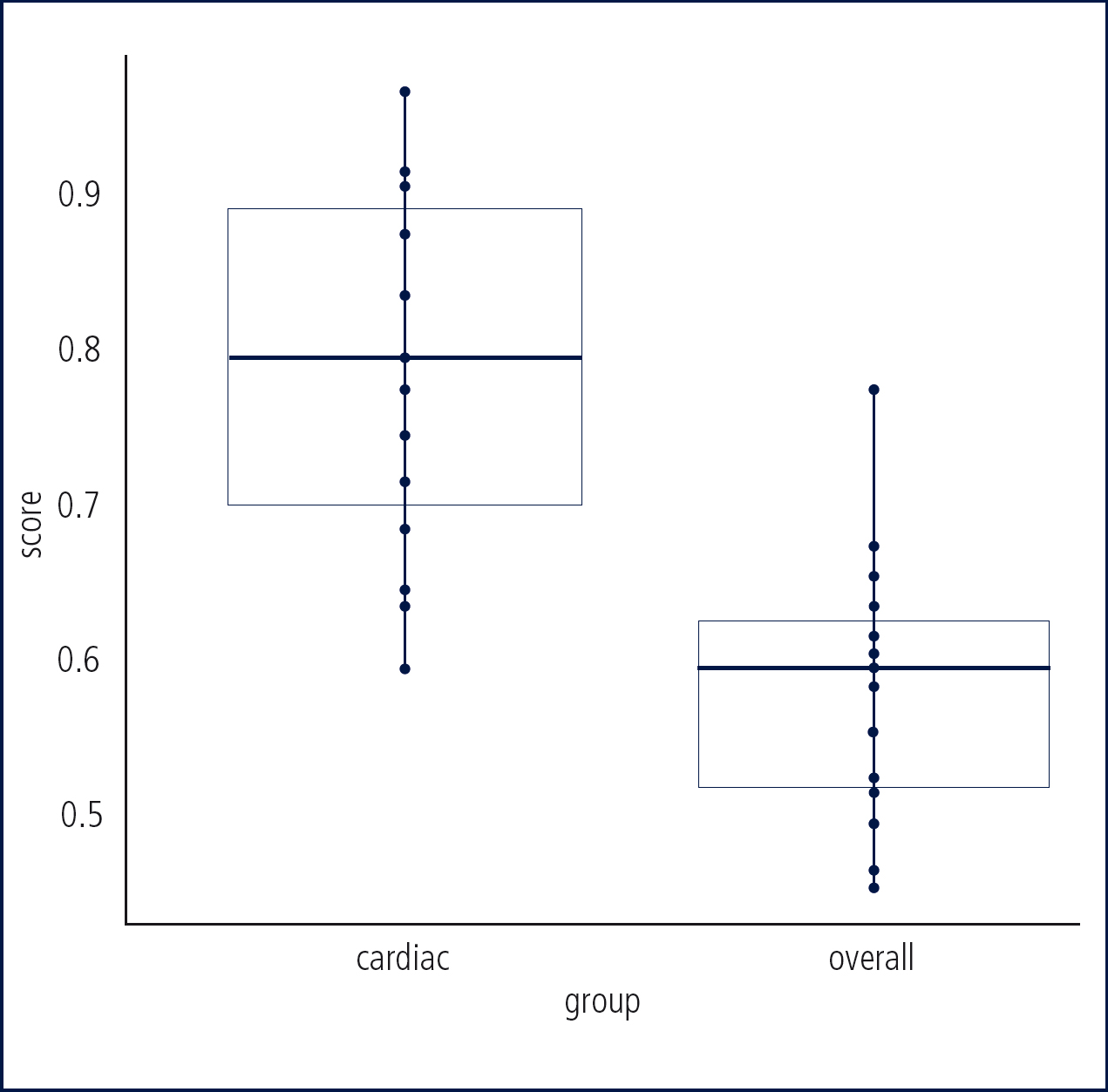
The mean test result for the 19 students who completed the cardiovascular unit was 78.5% (SD=11.5%) while the mean test result for the overall 12-week module was 57.5% (SD=8.3%) (Table 1). The differences were statistically significant, showing better results for the students in the unit with VR exercises (p<0.001) (Figure 3; Table 1).
| Test scores | ||||
|---|---|---|---|---|
| Mean | SD | Interquartile range | ||
| Cardiovascular anatomy test | 78.5 | 11.5 | 19 | |
| Year 1 anatomy & physiology overall module score | 57.5 | 8.3 | 10.5 | |
| t-test summary* | ||||
| t | df | p-value | Mean of differences | |
| T test | -7.59 | 18 | p<0.001 | -0.2094737 |
Usability of VR teaching tool
The survey responses of the students are outlined in Table 2. The response rate was 15/19 students (78.9%). All but two of the respondents used the VR equipment. The majority of respondents, 86.66% (n=13; 2 neutral) agreed or strongly agreed that VR was a useful part of the PBL learning unit to bring anatomy to life. Similarly, 86.66% (n=13) thought VR made the anatomy more memorable.
| STRONGLY AGREE | AGREE | NEITHER AGREE NOR DISAGREE | DISAGREE | DISAGREE STRONGLY | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | n | % | n | % | n | % | n | % | n | |
| Ease of use | ||||||||||
| I found the virtual reality equipment easy to access and had enough time to use it. | 46.67% | 7 | 26.67% | 4 | 6.67% | 1 | 20.00% | 3 | 0.00% | 0 |
| I found the virtual reality equipment easy to use. | 40.00% | 6 | 46.67% | 7 | 13.33% | 2 | 0.00% | 0 | 0.00% | 0 |
| My tutor effectively demonstrated the use of virtual reality equipment. | 46.67% | 7 | 13.33% | 2 | 20.00% | 3 | 13.33% | 2 | 6.67% | 1 |
| My level of computing skills made it difficult for me to use the virtual reality material. | 20.00% | 3 | 13.33% | 2 | 13.33% | 2 | 40.00% | 6 | 13.33% | 2 |
| The virtual reality video can be reviewed more quickly than text (n=14 for this question) | 57.14% | 8 | 14.29% | 2 | 21.43% | 3 | 7.14% | 1 | 0.00% | 0 |
| Impact on learning | ||||||||||
| Virtual reality problem based learning exercises bring the anatomy to life. | 73.33% | 11 | 13.33% | 2 | 13.33% | 2 | 0.00% | 0 | 0.00% | 0 |
| Virtual reality problem based learning exercises make the anatomy more memorable. | 60.00% | 9 | 26.67% | 4 | 13.33% | 2 | 0.00% | 0 | 0.00% | 0 |
| The use of virtual reality helped me to relate the scenario to real-life experience. | 40.00% | 6 | 46.67% | 7 | 6.67% | 1 | 6.67% | 1 | 0.00% | 0 |
| I felt that it was easier to identify relevant information from text than the videos. | 33.33% | 5 | 13.33% | 2 | 46.67% | 7 | 6.67% | 1 | 0.00% | 0 |
| Impact on PBL tutorial | ||||||||||
| The use of virtual reality had a positive impact on the group discussion. | 26.67% | 4 | 46.67% | 7 | 13.33% | 2 | 6.67% | 1 | 6.67% | 1 |
Ease of use
As reported in Table 1, the students were largely in agreement that the VR equipment was easy to access and manage during the length of the PBL tutorial (agree: 26.67%; Strongly agree: 46.67%), and was easy to use (agree: 46.67%; Strongly agree: 40%). Two students found that their level of computing skills made it difficult to use the VR materials; they opted not to use the equipment during PBL and observed their peers. Over half of the students strongly agreed that the VR materials could be reviewed quicker than text (57.14%).
Impact on learning and PBL tutorial
The majority of students agreed or strongly agreed that VR PBL exercises bring the anatomy to life, make the anatomy more memorable, help relate the scenario to real-life experience and make it easier to identify relevant information from text rather than the videos. Two-thirds of students strongly agreed that VR had a positive impact on the group discussion (66.67%). The majority of students thought virtual reality did not slow the pace of the PBL session (86.66%).
Discussion
In this study, the authors have demonstrated the design of a VR 3D anatomical model of the heart for cardiovascular education. When implemented in a PBL tutorial setting, the paramedical students in the present study had improved knowledge acquisition of cardiovascular anatomy and physiology compared with their performance on a non-VR PBL anatomy test. These results are aligned with evidence from fields other than paramedicine where VR reportedly improved knowledge acquisition in anatomy (Nicholson et al, 2006; Hampton and Sung, 2010; Tan et al, 2012; Drapkin et al, 2015; Kockro et al, 2015).
Although the authors did not have a large enough sample to have a control group of students, VR models appear to be valuable teaching tools in a variety of medical domains, which involve complex 3D relationships, such as molecular biology, immunology, and non-biomedical areas (Richardson et al, 2013).
Learners’ satisfaction after experiencing VR in the PBL tutorials was high. This evidence is aligned with other studies that show increased student enjoyment in 3D compared with 2D anatomy (Keedy et al, 2011; Drapkin et al, 2015; Kockro et al, 2015). A previous review emphasised the importance of experiences where learners are active participants, not passive bystanders (Issenberg et al, 2005).
Implementing VR in a larger cohort may mean that not all students have access to 3D equipment. However, the use of accessible anaglyphic 3D videos alone have been found to be insufficient in promoting learning (Goodarzi et al, 2017). The degree of interaction a student has with the VR environment may be important in knowledge and skill outcomes, and therefore warrants further investigation.
Regarding the hypothesised challenges of implementing VR in the classroom, the majority of students reported that VR equipment was easy to use. VR use in the PBL tutorial neither shortened nor lengthened the time to deliver the material. With regards to social dynamics, the authors found that it improved the group case discussion in a PBL setting. Previous studies compare VR to other digital learning and traditional didactic learning (Kyaw et al, 2019), rather than a PBL classroom.
Two students found their level of computing skills made it difficult to use the VR materials, which could be a barrier to VR use. For VR use to become a repetitive practice that is standardised in education, addressing students with physiological, cognitive deficiencies will be necessary. This may be why a dose-response effect has been reported elsewhere in using computer-aided learning to improve spatial reasoning (Guimarães et al, 2019).
The strengths of the study are the well-defined learning outcomes associated with the cardiovascular anatomy unit under evaluation. The study design is limited by small paramedic class size leading to a small sample size and absence of a control group. It is possible that the novelty of the 3D model may have encouraged the group to spend more time concentrating on the material than with the other modules, thereby leading to better test scores. One could argue that, either way, the outcome is the same: better understanding of 3D anatomical relationships. Another limitation of the current study was that it assessed short-term knowledge retention without directly assessing spatial understanding.
These preliminary findings demonstrate a swift and successful integration of a 3D virtual reality lesson in the programme. In this instance, the authors spent 8 weeks developing the 3D cardiovascular model evaluated in this study (excluding the hundreds of hours spent writing the software used to generate the 3D model).
Future studies should include a measure of the cost-effectiveness of interactive computer-based 3D environments. Moreover, paramedic education provides opportunities for further exploration of the use of synergistic teaching strategies such as the combination of simulations with 3D VR settings.
Conclusions
The present study investigated the impact of VR exercises on students' performance in anatomy examinations. The findings suggest that learners' cardiovascular anatomy knowledge acquisition can be improved through the addition of 3D VR exercises and VR use was acceptable to students. When delivered in a PBL tutorial, it was found to improve discussion.
Given that VR is growing in use and very few studies have attempted to describe its implementation and impact, the results of this study are positive in favour of VR use and need verification in larger extended studies. There is the potential for developments in 3D VR to be integrated further into health professions training.
