One of the goals of the Emergency Medical Services Chiefs of Canada (Emergency medical servicesCC), as defined in The Future of Emergency medical services in Canada: Defining the New Road Ahead (Emergency medical servicesCC, 2006) is to ‘mobilise health care. This is defined as ‘creating innovative models of service delivery to meet community-defined needs’ (Emergency medical servicesCC, 2006; The Community paramedic Program, 2009). Collaboration of emergency medical services and community organisations such as primary health care providers, social service agencies, and public safety groups can enable innovative initiatives that have the potential to improve the level of health-care within a community and reduce system pressures. The unique mobility of Emergency medical services can lead to the provision of primary health care by paramedics at the place and time where citizens need it, providing services according to the scope of practice determined and required by each community (Emergency medical servicesCC, 2006; Blacker et al, 2009).
Currently, high performance Emergency medical services systemergency medical services have health resources positioned for rapid response but are not always delivering emergency patient care. The use of these units can be optimised to provide primary care, as well as emergency services. Rural Australian paramedics have the opportunity to integrate with other health-care providers when they are not responding to emergency calls (O'Meara et al, 2007). Paramedics can contribute to health care when not participating in emergency responses, thus improving integration with community stakeholders (Stirling et al, 2007).
Community paramedicine is defined as a model of care whereby paramedics apply their training and skills in ‘non-traditional’ community-based environments outside the usual emergency response/transport model (Emergency medical servicesCC, 2006). The community paramedic may practice within an expanded scope by applying specialised skills/protocols beyond that which he/she was originally trained for. Alternatively, the community paramedic can practice in an expanded role, working in non-traditional roles using existing skills (International Round of Commuinity Paramedic (IRCP), 2011). An example of the expanded role includes the Long and Brier Island Project in the Province of Nova Scotia, Canada, which established a community partnership between the paramedic service and primary care agencies that dramatically altered the traditional work of paramedics (Martin-Misener et al, 2009).
Background
One of the current issues facing the health care system in the province of Ontario is the inappropriate use of acute care beds. The Ontario government created 14 Local Health Integration Networks to plan, integrate and fund local health services in each region of the province.
[The] aim of the Champlain Local Health Integration Network is to help coordinate health services so that people receive the care they need and deserve in a timely way. The Local Health Integration Network (LIHN) does not provide services directly. Rather, the mandate is to ensure that services are well organised, appropriately funded and meet the needs of residents of all ages'
The LIHN reported that the use of acute beds was not being optimised because the beds were being occupied by patients that should be in an alternative level of care bed. The average alternative level of care occupancy rate in acute care beds continues to rise (LIHN, 2006). A significant number of these patients could return home assuming adequate community supports and therefore potentially decrease the inappropriate use of acute care beds in Ontario hospitals. In response to these issues facing our current Health Care System, the Government of Ontario launched the Aging at Home Strategy. The purpose of this strategy is to allow seniors to live with dignity and independence in their own homes (LIHN, 2008; Lum, 2009). One of the initiatives developed out of the Local Health Integration Network Aging at Home strategy is the 24-hour flexible in-home support housing (Champlain LIHN, 2010). Services for these high-risk seniors include 24-hr urgent/on-call response, security checks, reassurance services, 24-hr pre-scheduled services (seven-days-a-week, 365-days-a-year), immediate medical and trauma emergency response, personal support and homemaking, and care coordination. These assisted living services are provided in part through collaboration between North Renfrew Long Term Care and the County of Renfrew Paramedic Service.
Methods
Study design
This study was a retrospective case series study that involved reviewing program charts of clients that participated in the LHIN ‘Aging at Home’ 24-hour flexible in-home support housing program located in a rural community, in the province of Ontario between 1 January 2010 and 30 April 2011. Either a community paramedic or personal support worker responded to each client medical or trauma incident. The request for assistance was generated by an alarm activated system, which the client used.
Primary outcome
The purpose of this paper is to review whether the use of community paramedics as part of an integrated health care team, can support clients living at home, resulting in a decrease in the use of 911 calls. The primary outcome is to measure the use of 911 activations.
Setting
The Aging at Home program in situated in the town of Deep River, part of the County of Renfrew, which encompasses 17 lower tier municipalities and one City. It had an area of approximately 770 000 hectares and a population of 97 454 in 2006 (Statistics Canada, 2011).
The County of Renfrew paramedic service is challenged by its vast geography and unique population settlement patterns and continuously adjusts its service delivery plan in an attempt to improve response times throughout the county. In 2011, the service responded to just fewer than 19 000 emergencies of which 66% were code 4 life-threatening calls (County of Renfrew, 2012). Close to 60% of all calls were used by patients over the age of 60 years-of age and 27% of all calls were used by patients over the age of 80 years-of-age (County of Renfrew, 2011). The catchment area is over 9000 km2 with a population of 120 000, expanding to 150 000 for the summer cottage season (Statistics Canada, 2011). The service continues to meet the community demand for non-emergency transfers and inter-facility transfers which also impacts its ability to respond to emergency calls in the rural communities.
The County of Renfrew assumed direct responsibility for the provision of land ambulance services on 1 January 2005. The service's current model is an advanced life support provided by Advanced Care and primary care paramedics staffing seven vehicles 24 hours a day, 7 days a week deployed from seven leased Ambulance Base Stations located in Arnprior, Barry's Bay, Chalk River, Eganville, Pembroke, Petawawa and Renfrew. An additional three vehicles operate 12 hours a day, 7 days a week to address the increased call volume during daytime hours.
The County of Renfrew Ambulance Service call volume for high priority calls has increased by about 18.8% average over the past six years. Conversely, the call volume for low priority calls has decreased by about 50.9% over the same period (Ministry of Health and Long-Term Care, 2010). The service has experienced a mean average call volume for the last six calendar years of 17 108 each year.
The telephone number used in the Canada to call the emergency services is 911 and is part of the North American Numbering Plan. Similar to 999 in the UK and 000 in Australia, the telephone number provides the public with rapid access to communication centres, which are linked to paramedic service providers via radio networks.
Intervention
Access to the Aging at Home program is defined by the provincial government. Candidates eligible to participate in the program must be both on the waiting list for a long-term care bed and be able to remain at home while waiting to be placed. When an opening occurs in the program, the person on the top of the list is offered an opportunity to join the program.
Each client participating in the program is introduced to the call-bell system, which provides direct contact between the client and the paramedic or personal support worker. Direct contact is provided 24 hours-a-day. When a client is in any distress, the activation of the call-bell system alerts the paramedic or personal support worker. Either the paramedic or personal support worker responds to the clients' residence. The call-bell system is an Aging at Home program activation system and does not activate 911. The alarm activation can be manually accessible via bracelet, necklace, as well as automatic notification via door alarms, fire and smoke as well as moisture sensors. The local dispatch centre does not have any contact and cannot assign any local emergency call to the community paramedic.
While the Aging at Home program runs 24 hours-a day, the County of Renfrew Paramedic Service actively participates for 32 hours per week, which consisted of shifts from 1100–1900 hrs Monday, Wednesday, Friday and Saturday of each week. Each medical/trauma incident managed by a community paramedic is a primary care paramedic (Paramedic Association of Canada, 2001). During each shift, the Community paramedic may be partnered with a Personal support worker or may work independently depending upon the needs of the clients in the program. Throughout the duration of the study period, the community paramedics used the primary care paramedic scope of practice in order to respond, assess and treat the clients participating in the program. The community paramedics used first response equipment in a non-emergency Ford Escape in the event the client required acute medical or trauma intervention. In some responses, the community paramedic may use the vehicle to transport the client to either the physician office or the local hospital emergency department.
The paramedics expanded their role in the program by gaining additional hours of instruction on fall prevention, home safety assessment, urinalysis, diabetic assessment education, wound care, dementia awareness, acquired brain injury communication strategies, basic physiotherapy exercises, as well as health promotion activities. In order to improve communication with clients who experience dementia, paramedics required additional communication instruction. The better understanding of how the client processes information and the use of communication strategies improved the ability to establish baseline behaviour and health. Basic physiotherapy exercises also allowed for the opportunity to evaluate the client and determine what aches and pains were chronic in nature. Medical oversight of the program is provided by the Regional Paramedic Program of Eastern Ontario. The decision to have the client transported or remain at home was made solely by either the community paramedic or personal support worker. The community paramedic established direct physician contact for referral options. When urinalysis assessment, and wound care assessment and treatment were required by the client, the results were shared with the physician. This allowed the physician to communicate the next steps in the health care plan for the client. The added benefit was a decreased number of visits to either the emergency department or physician's office.
‘The better understanding of how the client processes information and the use of communication strategies improved the ability to establish baseline behaviour and health’
Data collection
Two investigators (MR, AS) transcribed each medical or trauma response attended by either a community paramedic or personal support worker into Microsoft Word and Excel datasheets. Within each response, the name of the client, date of the incident, description of the chief complaint, and whether transportation to the hospital emergency department was facilitated by using 911 was reviewed.
Analysis
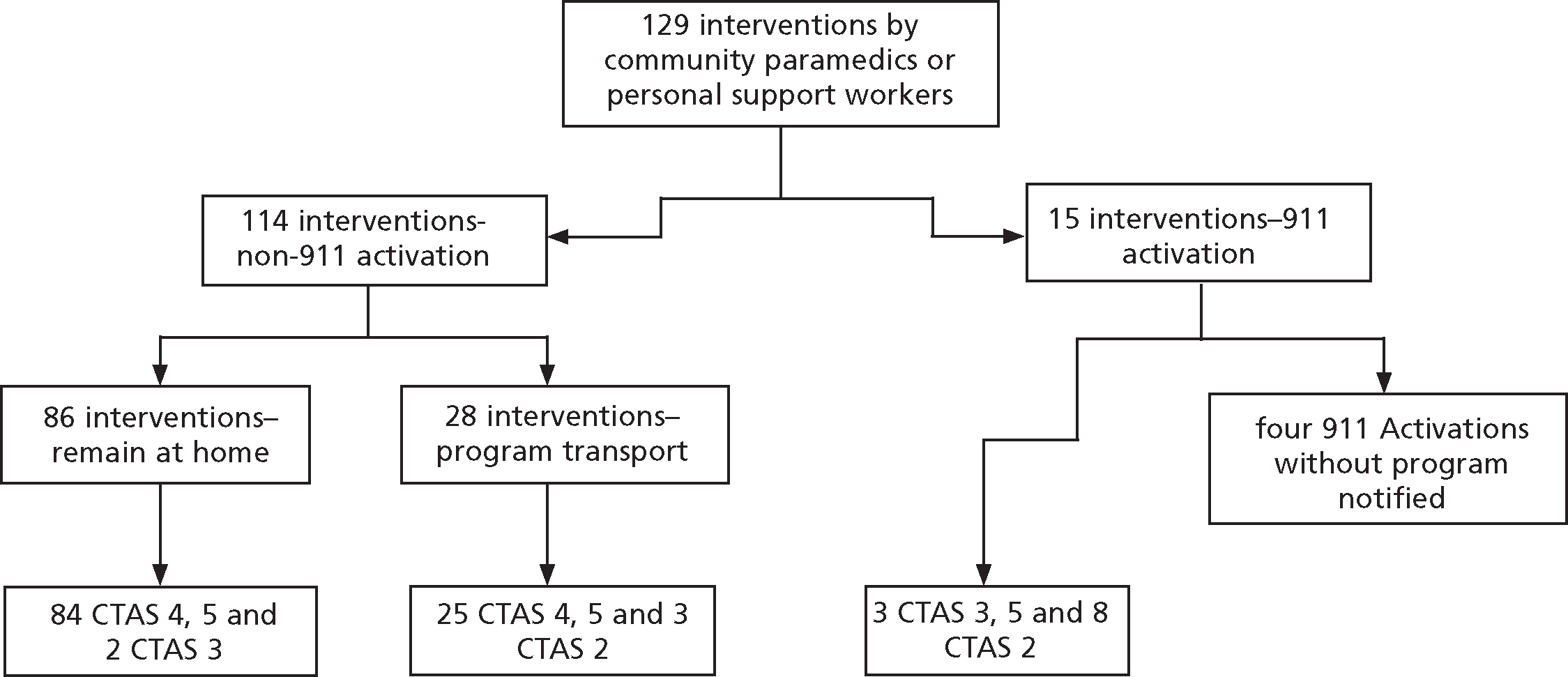
The total number of interactions with the clients was 129. Of the 129 interactions, 114 did not require the use of 911 with the remaining 15 using 911 and the County of Renfrew Paramedic Service for the transport of the client to the local emergency department. Of the 114 interactions not requiring the use of 911, 86 remained in the home of the client. The CTAS (Canadian Triage and Acuity Score) score of these 86 interactions were further broken down to two interactions with a CTAS 3 score and 84 interaction with a CTAS 4–5 score. The clients that were transported by the County of Renfrew Paramedic Service had CTAS 2 scores for eight of the calls and CTAS 3 for three calls. There were five clients that required community paramedic attention more than ten times each during the study period. A total of 61 interactions representing 47% of the total 129 interactions were requested by the five clients. The most common chief complaint was falls (40%). The number of return visits to the local emergency department in 28-day period was 8%.
To ensure that the decision not to use 911 by either the community paramedic or personal support worker did not put the client at risk, hospital emergency visit and admission records were reviewed 28 days after the initial medical or trauma response by the community paramedic or personal support worker. The decision not to use 911 by the community paramedic or personal support worker was measured against either an emergency department visit or admission during the 28 days. Attendance to the client on day 0 was combined with any unplanned emergency department Visits or hospital admissions in the 28 days that followed to provide information on the care provided. Ethical approval for this study was obtained from the Deep River Hospital Ethic Board.
Results
Over the sixteen months, 27 clients were enrolled in the study. The study included residents aged 69–94 years of age, with an average age of 85 years and a median age of 87 years. Of this elderly population, 17 (54%) were women. The distribution of the interactions was 57% medical calls versus trauma calls with 59% of the interactions involving female clients. All 27 clients resided in one or two storey homes dwellings, as well as low rise apartment buildings. Data were available for 100% of 129 medical/trauma incidents. The two investigators coded the chief complaints into 13 categories (Table 1). The categories were established as the interactions were reviewed. The reviewers coded the chief complaints independently. A review of the differences was marshalled by the third researcher (CD). The inter-ratters reliability achieved a per cent of overall (observed agreeement/Po of 0.968993 and a free-marginal kappa score of 0.966409.
| Medical/trauma incidents as documented by community paramedics or personal support workers | Number of occurrences | Percentage of occurrences | Received intervention | Number of incidents transported to the emergency department | Number of incidents transported to the admitting department | Number of ED Visits post 28 days |
|---|---|---|---|---|---|---|
| Falls | 51 | 40% | 29 | 3 | 0 | 4 |
| Anxiety | 15 | 12% | 15 | 0 | 0 | 0 |
| Generally unwell | 14 | 11% | 13 | 4 | 4 | 0 |
| Genitourinary | 8 | 6% | 8 | 3 | 2 | 0 |
| Gastrointestinal | 8 | 6% | 7 | 1 | 1 | 3 |
| Neurological | 7 | 5% | 6 | 3 | 0 | 0 |
| Social | 6 | 5% | 4 | 0 | 0 | 0 |
| Cardiac | 6 | 5% | 6 | 2 | 2 | 0 |
| Wound care | 4 | 3% | 4 | 2 | 0 | 0 |
| Medication compliance | 3 | 2% | 3 | 0 | 1 | 0 |
| Syncope | 3 | 2% | 2 | 0 | 0 | 0 |
| Environmental | 3 | 2% | 1 | 0 | 0 | 0 |
| Cardiac arrest | 1 | 1% | 1 | 0 | 0 | 0 |
| Total | 129 | 100% |
Of the 129 medical or trauma client interactions identified in the study period, 86 end results saw the client remaining at the home because of community paramedic or personal support worker intervention and therefore, neither 911 activation nor emergency department visits were required Figure 1). An additional 28 interactions resulted in the transport of the client to the emergency department but without activating 911. In these 28 interactions, the client was transported to the emergency department using the program vehicle. All of the transports to the emergency department were facilitated by either a paramedic or a personal support worker. Finally, an additional 15, representing 12% of the interactions required a call to 911 to have an ambulance transport the client to the emergency department.
Falls accounted for 40% of interactions. A review of the data revealed that all the falls occurred in the kitchen, bathroom or bedroom. Of the 51 interactions, 48 clients were assessed and treated without the need of 911 or Emergency Department resources. In another 15 interactions, clients experienced anxiety episodes. Each of the anxiety episodes were defused through the assessment of the client followed by ensuring the provision of the client's safety in their home. In an additional 14 interactions, generally unwell clients were monitored for fluid intake while managing both nausea and vomiting.
The next set of interactions involved the management of clients that experienced either urinary tract infections or urinary retention difficulties (eight interactions). The ability to perform urine analysis, assess for urinary retention and refer to the family physician for medical follow up diverted these patients from the hospital emergency department. The next category made up an additional 6% and includes gastrointestinal problemergency medical services. The gastrointestinal problemergency medical services include either incontinence urine or faeces or bowel obstruction.
With each incident, either the community paramedic or the personal support worker were first to arrive to the resident, had the opportunity, in all but four interactions, to assess the patient. Further, the activation of 911 and request the assistance of a transporting paramedic crew could be initiated if required. In the interactions where transport was required, the determination for paramedic transport to the emergency department was based upon the client's required care needs being beyond the capacity of the community paramedic or personal support work.
In the case of the four additional 911 activations and visits to the emergency department, each of these occurrences was initiated by family members for the clients of the program. The program was made aware of the 911 activation and emergency department visit after the occurrence.
A total of 71 clients presented themergency medical serviceselves to local hospital during the study period. Of the 71 visits, 48 were emergency department visits and 23 were admitted as inpatients. Of the 48 emergency department visits, 28 were transported by the program, 13 by the County of Renfrew Paramedic Service, and seven were follow up appointments. When reviewing the required use of 911, the incidents involved sepsis, pneumonia, lower back pain, unresponsiveness, dislocation of the knee, shortness of breath with tachycardia as well as a Foley catheter removal resulting in uncontrolled bleeding. The number of return visits to the local emergency department in 28 day period was 8%. All of the follow up appointments were associated with the 41 original emergency department visits. There were no emergency visits or hospital admissions as a result of the non-transport interactions completed by either the community paramedic or personal support worker.
Discussion
The result of this retrospective analysis demonstrates that during 86 incidents, which consisted of 84 CTAS 4 or 5 and two CTAS 3 scores, safe care was provided without the use of 911 and the emergency department resources. The Canadian Triage and Acuity Scale is divided into five triage levels:
As stated by Bigham et al (2011), ‘[with] the diverse scope of practice, many have suggested paramedics may be well suited for treating patients with minor conditions in the field or referring them to nonemergency department health resources. Mason et al (2007) state that with a treat and refer program, ‘paramedics can be trained to see and treat people with minor conditions and reduce the need for emergency department attendance’. The result could be treating the right patients in the right place at the right time. In addition, clients find this approach more satisfactory than attending the emergency department (Woollard, 2006).
A number of studies have evaluated the safety of the client when care is provided by paramedics by assessing the unexpected visits to the emergency department or admissions after the assessment and treatment provided by the paramedic has been completed (Mason et al, 2007, 2008). After reviewing our findings, there is additional support for the suggestion that paramedics can make safe decisions regarding patient care needs in the community. The decision not to use 911 was validated by reviewing the hospital records for unplanned hospital visits and admissions for the clients of the program in the 28 days after the initial episode. Each intervention was reviewed by chief complaint and cross referenced for any emergency department visit or hospital admission.
Limitations
We assessed a single integrated team in northeastern Ontario, which limits the extent to which the results can be generalised to other programs. In addition, this study is limited by sources of error common to all retrospective chart reviews, such as incorrect recording of data on the initial log, incorrect transfer of data, missing data on the log, and inconsistent interpretation of the logs. The creation of the categories had a high inter-raters reliability rating between the two evaluators. This high rating may be a bias as a result of the two evaluators being of the same paramedic service working in the same geographical and cultural area.
Each client interaction record reviewed did not indicate whether a paramedic or personal support worker lead in the assessment and treatment. The limited number of interactions may make generalising these results to other settings challenging. In addition, the question of whether all clients seen by community paramedic or personal support worker would have called 911 if this new service was not implemented for every interaction can be challenged.
The implicit design of retrospective case series studies excludes the use of a control group and cannot take advantage of a before-after or time series research design, and therefore exposes this study to internal validity challenges. Internal validity could include maturation. As the program participants grow older and the medical challenges become more complex, the demands for interactions will increase. The increased frequency of visits may not be transferable to an avoidance of a 911 call. Instrumentation is another potential internal threat to validity. The documentation process changed during the research time period. This change could affect the effectiveness of the documentation of interactions.
Future direction
Shah et al (2010) makes the observation that gives a clear demonstration of this program the improvement of quality of life for seniors. They can remain safe and at home through the use of local collaboration of existing services. This study involving community paramedics creates the impetus for a number of interactions that may be worth considering. Additional research opportunities exist with the Aging at Home program.
First, a comparative study where data collected would compare the 36 hours covered by the paramedic versus the hours covered by the personal support worker would provide an opportunity to evaluate the community paramedic contribution in isolation. A review of the number of 911 activations during the paramedic shifts could demonstrate the exact contribution of the Community paramedic versus the Personal support worker in the reduction in use of 911. Second, as (2004), Dixon (2009) and Martin-Misener et al (2009) suggested, there may be cost savings avaiulable with community paramedicine. This study was unable to analyse these results but future studies should be developed to quantify the potential savings to Emergency medical services and the emergency department. Third, the need to report on the satisfaction of the clients is required. A satisfaction survey similar to the ‘The Common Measures Tool’ criteria defined in the Toward Citizen-Centred Service Delivery: A How-To Guide for the Service Improvement Initiative (ICCS (Institute for Citizen-Centred Service) 2007) should be considered. The criterion includes timeliness, knowledge, extra mile, fairness, and outcome and could contribute to the overall satisfaction of community paramedic contribution to the primary care arena. Fourth, the needs of the clients demonstrate a requirement to increase the knowledge base of the health care system, as well as an expanded scope of knowledge, skills and attitudes of community paramedics in order to meet the health care needs of the client in each community (Woollard, 2006; Blacker et al, 2009). Research may also be required to validate whether this knowledge and skills is best provided in an organised and recognised format of a post graduate program (Mason, 2003; Blacker et al, 2009) or a self directed paramedic service delivery program. In order to establish professionalism and high quality patient care, consideration for standardisation of competencies of community paramedics may be required (Woollard, 2006). The Paramedic Association of Canada is the home of the Canadian National Occupational Competency Profile, which currently defines competencies for emergency medical responder, primary, advanced and critical care paramedics but does not include a community paramedic profile (Paramedic Association of Canada, 2011).
Finally, looking for opportunities to integrate health services in partnership with other health professional to promote disease and injury prevention is required (Blacker et al, 2009). Research that reports on the integrated care may provide valuable information on the best approach to ensure coordinated provisions of care (O'Meara et al, 2007). Patient- or client-centred guidelines can only be attained by a multi-professional designed approach that allows the client to receive ongoing care within the community (Integrated care, 2005; Mirando et al, 2005).
Conclusions
This study implies that the contribution of the community paramedic in the Aging at Home program can contribute to the reduction in 911 activations without compromising the health of the clients. This paper acknowledges that the impact analysis of 911 activations is only one way to evaluate the contribution of the community paramedic in a 24 hour flexible in-home support program by a multidisciplinary health care team. The study also suggests that additional research can further validate the community paramedic contribution through the use of a comparative study. In addition, there is an opportunity to explore the questions of potential system financial savings; defining community paramedics core competencies, and determining the level of satisfaction of the clients.
