Coronaviruses are responsible for many viral respiratory diseases in both humans and animals (Giwa and Desai, 2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes the disease COVID-19, is a novel strain of coronavirus first identified in humans in December 2019 in the Wuhan province of China (Chan et al, 2020). As with previous coronaviral strain outbreaks such as Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) coronavirus, transmission is believed to be via respired droplets and fomites (Sohrabi et al, 2020; Wong et al, 2020).
The virulent spread of COVID-19 globally has led to the World Health Organization (WHO) declaring it an international emergency (Sohrabi et al, 2020), draconian social restrictions resulting in economic standstill, mass paranoia and a death toll of over 80 000 within a few months (WHO, 2020).
At the onset of the pandemic, there was understandably a paucity of published research on COVID-19, which was of concern to healthcare providers, governments and the public. A lack of rigorous evidence and knowledge upon which to inform a response to COVID-19 may lead to fear, confusion and panic, as seen during various pandemics throughout time (Pfefferbaum and North, 2020).
Although much remains unknown, frontline health professionals such as paramedics, nurses and doctors have to continue to treat patients. It could be argued that extra pressures and stresses affect practitioner mental health, which may impact working efficiency and the capacity of the NHS (Greenberg et al, 2020). News reports suggest that medical services are under strain with resourcing and personal protective equipment (PPE) shortages (Glauser, 2020; Ranney et al, 2020).
Many students qualified and registered early as health professionals and various volunteer schemes were created to support the NHS services (Haines et al, 2020; Mahase, 2020; NHS England, 2020). How adequate their preparation for their professional roles, both mentally and clinically, may be challenged.
Research on practitioners' attitudes during the COVID-19 outbreak is lacking while numbers of staff falling ill, self-isolating or failing to attend shifts because of fear may continue to rise (Misra, 2020).
Investing in measures to ensure staff resilience and therefore capacity in frontline healthcare is paramount in preparing for a pandemic (Martland et al, 2020). Ensuring mental health and wellbeing are supported during these stressful times is key (Greenberg et al, 2020).
This paper aims to review the literature on frontline practitioners' experiences during a pandemic, drawing findings from previous viral epidemics caused by the viruses in the same family, notably the MERS outbreak in Korea in 2015 (Oh et al, 2018) and SARS in 2003 (Chong et al, 2004).
Methods
Search strategy
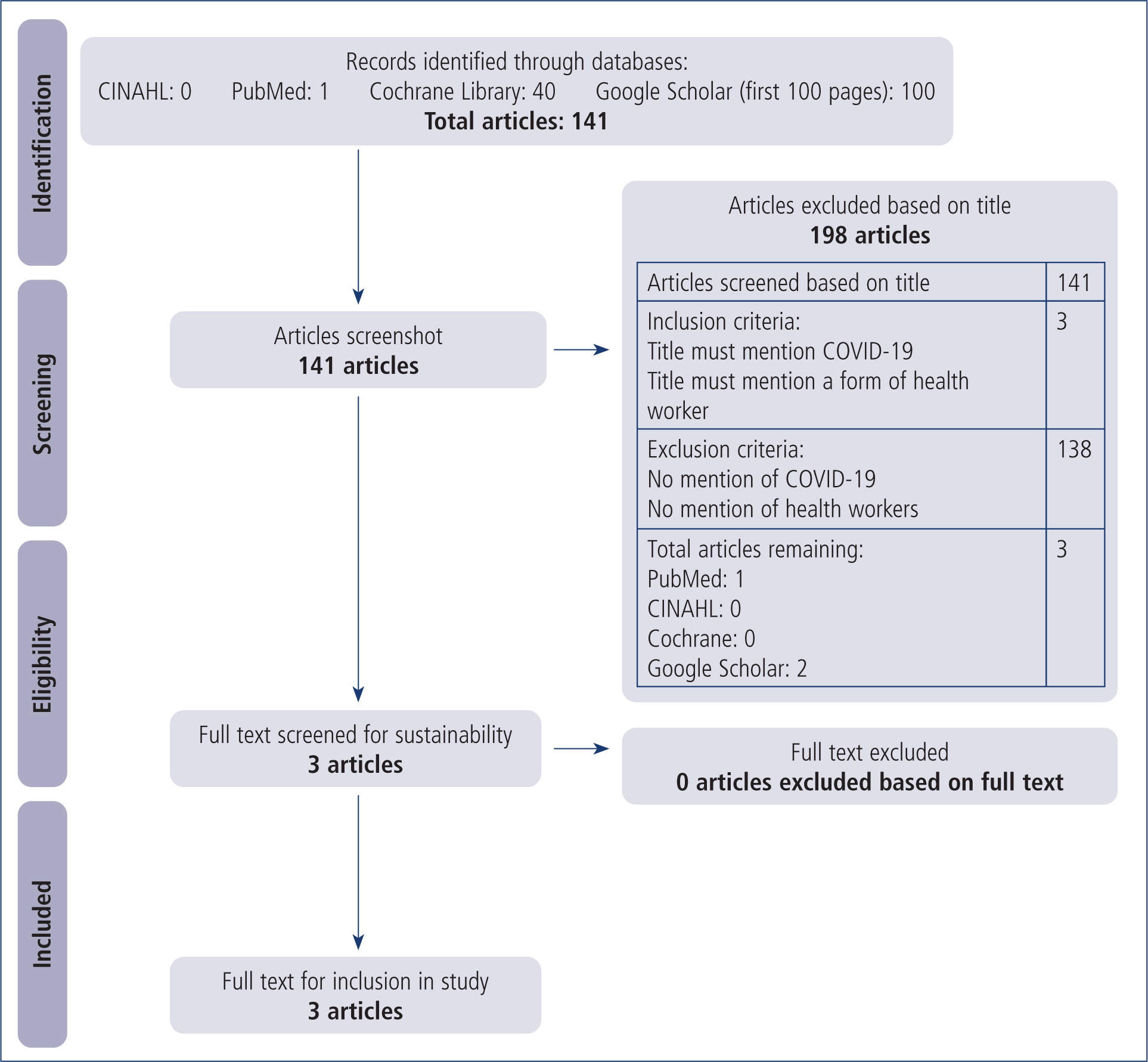
The authors carried out a literature search on 23 and 30 March 2020 using the Cochrane Library, PubMed and CINAHL. Google Scholar was also used to find grey literature around pandemics, national responses and preparedness of practitioners. The MeSH terms ‘allied health personnel’, ‘emergency medical technician’ and ‘COVID-19’ were used to keep the search terms broad.
Although an attempt was made to conduct a systematic review of current literature, there was so little work published concerning COVID-19 and health professionals' experiences at the time of writing that literature on past epidemics and frontline workers' attitudes was sourced through Google scholar and by studying reference lists of relevant articles to create context for this study.
As a result, a scoping literature review is presented. Google Scholar was searched using the terms ‘COVID-19’, ‘healthcare’, ‘paramedic’, ‘experience/attitude’ and ‘epidemic’ to build up a bigger contextual picture of frontline workers' attitudes during a pandemic. Reference lists were assessed by title for articles with the MeSH terms or search terms above.
All studies used were assessed for quality using the GRADE-CERQual confidence rating system for qualitative data analysis (Lewin et al, 2018) (Appendix 1). Articles that did not involve primary data sourcing were also assessed and noted if GRADE-CERQual was not applicable.
Results
The authors used the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Moher et al, 2009) and screened articles by their title, according to inclusion and exclusion criteria (Figure 1). Of 141 results, three met the inclusion criteria, and were included in the study.
Searching Google Scholar as well as reference lists provided a much wider dataset of 18 articles (Appendix 2).
Of all the papers, only two were from British research (Ives et al, 2009; Greenberg et al, 2020) (Box 1). Seven were specific to the COVID-19 outbreak, seven were in relation to the SARS outbreak and four were written in reference to influenza outbreaks or potential epidemics. Only three papers specifically referred to responders (Mackler et al, 2007; Glauser, 2020; Townsend and Eburn, 2020), and 10 studies concerned hospital settings. Five papers were inclusive of all health professionals.
| Article origin | |
| Britain | 2 |
| America | 4 |
| Canada | 4 |
| Singapore | 3 |
| China | 2 |
| Australia | 2 |
| Taiwan | 1 |
| Disease | |
| COVID-19 | 7 |
| SARS | 7 |
| MERS | 0 |
| Influenza | 4 |
| Practitioner | |
| First responder/paramedic | 3 |
| Hospital practitioners (nurses/doctors) | 10 |
| Health workers in general | 5 |
Nine papers were written following surveys and qualitative studies (Cheong et al, 2004; Chua et al, 2004; Poon et al, 2004; Straus et al, 2004; Mackler et al, 2007; McAlonan et al, 2007; Tam et al, 2007; Ives et al, 2009; Seale et al, 2009). Three studies retrospectively considered previous epidemics to assess current resilience (Tiong et al, 2013; Greenberg et al, 2020; Ho et al, 2020). One study considered current standards of in-hospital care and efficiency during COVID-19 (Wong et al, 2020). Three papers concerned specific healthcare settings to examine changes in working practices during the current pandemic—cardiovascular ward (Driggin et al, 2020), paramedic ethics (Townsend and Eburn, 2020) and intensive care nursing staff (Martland et al, 2020)—considering resource management, communication and appropriate PPE.
Discussion
Several themes were identified through the findings, such as frontline workers being considered a high-risk group and practitioners' main concerns that influence work attendance and mental health. Staff confidence in PPE appears to impact their mental resilience. These topics will now be expanded upon.
Risk to frontline workers
It is well documented that frontline workers are at a higher risk of infection and, that in past epidemics such as SARS and Ebola outbreaks, were the most frequently infected after providing care to primary victims (Chong et al, 2004; Huber and Wynia, 2004; McAlonan et al, 2007; Ho, 2020).
This is also the case for COVID-19 as supported by Driggin et al (2020). Wang et al (2020) found that, of the 138 patients in their dataset, 40 were practitioners who had contracted the disease in a hospital environment. Wu et al (2020) found that 1716 of 44 672 patients in their study were health practitioners. The first three COVID-19-related deaths of doctors in the UK were announced in the first week of April (British Medical Journal, 2020).
Practitioner concerns
Apprehension around infecting family members appears to be the biggest driver of fear (Chong et al, 2004; Chua et al, 2004; Mackler et al, 2007; McAlonan et al, 2007; Ives et al, 2009). Many workers feel conflicted by their professional duty of care and self-protection during epidemics (Straus et al, 2004; Seale et al, 2009; Tiong and Koh, 2013). Other concerns are unemployment, isolation, contracting the disease, mortality and fears that the job puts them at greater risk (Chong et al, 2004; Ho, 2020). Staff become very attentive to any changes in their body's performance, such as coughs and temperature fluctuations (Chong et al, 2004).
Natural anxieties during pandemics may lead to health professionals taking desperate measures to ensure the safety of their families, such as seeking other employment (Tam et al, 2007) or absenteeism, drastically affecting workforce capacity (Bonneaux, and Van Damme, 2006; Seale et al, 2009). A scarcity of research in this area means there are gaps in pandemic planning and frantic resource management (Mackler et al, 2007). There are also ethical conundrums when dealing with finite resources for unprecedented patient group sizes (Townsend and Eburn, 2020), and stress and guilt associated with these can lead to the development of mental health issues (Greenberg et al, 2020).
However, studies also highlight a tenacity shown by many professionals (Huber and Wynia, 2004). In an Australian study, Seale et al (2009) found that the majority of practitioners would continue to treat patients during pandemics. This is supported by Tam et al's (2007) study in Hong Kong, which noted that staff members who had experienced the SARS outbreak showed greater confidence when dealing with the concurrent avian flu epidemic. This demonstrates knowledge around personal care and mass casualty scenario management to be a beneficial coping mechanism (Wong et al, 2020). Better education around safeguarding themselves and families increases practitioners' confidence and willingness to take professional risks (Straus et al, 2004; Mackler et al, 2007). Practitioners felt united by the hardship and assurance increased with viral knowledge and understanding (Cheong et al, 2004; Chua et al, 2004).
Confidence in PPE
Frontline health services recognise that NHS staff are more exposed than the general population to the risks of contracting COVID-19 (Moore, 2020). Senior officials have advised that following health and safety guidance and strict infection prevention and control (IPC) measures can reduce employees' risks of exposure (Moore, 2020). However, PPE should be the last defence in the line of precautionary measures that an organisation should take to ensure staff safety according to research (Wong et al, 2020; WHO, 2020; Health and Safety Executive, 2020; Martland et al, 2020).
Both WHO and the United States Center for Disease Control and Prevention (CDC) (2020) recommend IPC measures for contact and droplet protection (Giwa and Desai, 2020), and recommend airborne precautions during procedures at risk of generating aerosols such as intubation or cardiopulmonary resuscitation (Driggin et al, 2020; WHO, 2020).
Confidence in effective PPE is noted to lessen anxiety in practitioners even more than a vaccine alone (Mackler et al, 2007), compounding the importance of availability and assurance in effectiveness. According to WHO (2020), staff should be monitored for compliance, PPE supply should be adequate to meet needs, decontamination of vehicles should be consistent and levels of COVID-19 among practitioners should be monitored. McAlonan et al (2007) found that 84% of their practitioners had confidence in their PPE. However, Seale et al (2009) noted that health staff considered their places of work to be insufficiently prepared for a pandemic.
IPC training must be regular, clear and consistent as the situation evolves, and management plays a key role in keeping staff updated, making them feel valued and listened to (Martland et al, 2007; Ives et al, 2009). Good communication throughout the workforce is vital in limiting transmission and ensuring adherence (Wong et al, 2020). Lack of clear communication and poor staff training have been noted to lead to post-traumatic stress disorder (PTSD), and Ho et al (2020) noted resolution of anxiety with the provision of good communication. Greenberg et al (2020) support this theory by noting that good communication from management and frank details of what to expect go some way to dampen the risk of developing anxiety and mental health disorders.
Practitioner mental health during a pandemic
A lack of research on the effects of COVID-19 on the mental health of frontline workers, specifically first responders, was noted at the time of writing.
The majority of studies from past epidemics use a demographic of hospital practitioners. Considering the outcomes of previous research, issues raised include ethical quandaries surrounding allocating limited resources (Tiong and Koh, 2007; Driggin et al, 2020) associated with feelings of guilt and disgrace. Other themes are depression, nervousness and tension (Chong et al, 2004), and the constant strain of anxiety leading to exhaustion, a lack of sleep and, ultimately, burnout (Seale et al, 2009). The level of stress experienced during a health crisis can lead practitioners down a route to developing depression, or PTSD (Greenberg et al, 2020).
Many paramedics have experienced mental health issues because of occupational exposure (Streb et al, 2014); these previous presentations of mental illness increase susceptibility to developing further mental health issues during these times (Ho et al, 2020; McAlonan et al, 2007).
Stress and trauma experienced now will contribute to mental health vulnerability after a pandemic and continue to affect resourcing, as was noted following the SARS outbreak and influenza epidemics (McAlonan et al, 2007; Seale et al, 2009). Research has demonstrated that following pandemics, health workers experience heightened anxiety and depression at levels much greater than the general public (Ho et al, 2020). This notion is supported by Greenberg et al (2020), who drew upon experience of previous pandemics to surmise that high levels of PTSD and mental health issues will affect workers following COVID-19. Tam et al (2007) also found variation in the degree of practitioner wellbeing depending on risk level.
Liu et al (2020) say that COVID-19's rapid impact has affected the mental health of China's practitioners and the nation. China released documents and online mental health support to aid during the mental health crisis now looming among practitioners and the public following the COVID-19 outbreak (Liu et al, 2020), as such support is known to affect workforce resilience (Ho et al, 2020).
Limitations
This article was written at the start of the pandemic and, because of the lack of published work available on practitioners' attitudes to the pandemic at the time, it has only been possible to perform a scoping literature review. A portion of work assessed was either not applicable for quality grading or deemed to be of low confidence, and no randomised control trials were found.
However, intense study has since been focused on COVID-19, which suggests the evidence base may have progressed beyond the realms of this paper. Another literature search was undertaken on 30 July 2020, using the same search terms as in this study, yielding 6353 results before any screening was undertaken (PubMed: 785; CINAHL: 5525; and Cochrane reviews: 43). This demonstrates scope for much larger and more specific systematic reviews moving forward.
Conclusion
The aim of this paper was to examine practitioners' attitudes to working during a pandemic as reported in the literature and identify any common themes.
Work published concerning previous viral outbreaks and practitioners' experience was used owing to a lack of literature specific to the COVID-19 pandemic.
The aim has been met through the identification of certain themes emerging from the research. This paper identifies that mental health of practitioners may be drastically affected during a pandemic (Greenberg et al, 2020). Health professionals' biggest concerns are around infecting family members (Chua et al, 2004) and the ultimate battle is overcoming personal anxieties to continue treating patients (Tiong and Koh, 2007).
The scarcity of research published concerning paramedics' attitudes during the COVID-19 pandemic highlights a lack of understanding around the mindset of these practitioners, and increases the risk of absenteeism, mental health problems and reduced resilience (Chong et al, 2005; McAlonan et al, 2007).
Several themes identified through the present study are suggestive in supporting mental health. First, practitioners should have a thorough understanding of the risks and how to protect themselves and their families (Mackler et al, 2007). Second, they should be confident about their PPE (Straus et al, 2004). Finally, good communication throughout a crisis is a vital in ensuring mental preparation and monitoring practitioners' mental health (Wong et al, 2020).
Sufficient foresight gleaned from surviving previous epidemics should encourage greater investment in research into this area as a stronger health service offers greater resistance to biological threats as they arise (Van Damme and Van Lerberghe, 2004; Bonneaux and Van Damme, 2006). It is also important to assess whether practitioners are left with post-traumatic effects after dealing with this pandemic, which may affect their resilience during a future epidemic (Tam et al, 2007).
The articles addressed in this paper are from all over the world. Only two are from the UK where the authors are based. This begs the question: what is the British practitioner mindset during this crisis? How is it affecting health professionals' attitudes to the workplace and what systems are in place to ensure mental resilience and a stronger NHS? Future investigation into this area is urgently required. This paper is also informing a qualitative study exploring paramedics' experiences of providing care during COVID-19.
