Clinical handover is an integral part of the daily clinical work that takes place between paramedics and emergency department (ED) staff for every patient arriving at the hospital by ambulance or helicopter. This area of transition of care, however, has been sparsely researched (Wood et al, 2014). An ineffective handover represents a breakdown in communication of health information, which in turn may have deleterious effects on patient care and safety, including: misdiagnosis or unnecessary delays in diagnosis (Kachalia et al, 2007); delays in administration of treatment; administration of incorrect treatment or medication errors; and omission of care (Joint Commission Centre for Transforming Healthcare, 2014).
This literature review deals with the clinical handover between paramedics and ED staff (physicians and nurses), specifically focusing on two frequently used patient handover acronyms and their effectiveness and limitations in facilitating a complete, concise, and structured clinical handover. The SBAR (Situation, Background, Assessment and Recommendations) and IMIST-AMBO (Identify, Mechanism/Medical Complaint, Injuries/Information related to complaint, Signs and Symptoms, Treatment and Trends—Allergies, Medications, Background, Other information) acronyms will be explored. Given the unique requirements of each discipline, this review does not take into account the clinical handover among ED staff between shift changes or the clinical handover between ED and other hospital departments (intensive care unit, medical, and surgical floors).

Definition
Handover is also referred to as ‘handoff’, but for the purpose of consistency, the word ‘handover’ will be used throughout this article.
Clinical Handover is ‘a real-time process of passing patient specific information from one caregiver to another or from one team of caregivers to another for the purpose of ensuring the continuity and safety of the patient's care’ (Joint Commission Centre for Transforming Healthcare, 2014: 2).
The primary objective of a clinical handover is the transfer and acceptance of professional responsibility and accountability of patient care among healthcare professionals (Joint Commission Centre for Transforming Healthcare, 2014). During this process, the information about a patient's care, treatment, current condition, and any recent or anticipated changes must be clear, complete, and accurate in order to minimise preventable deleterious events and to ensure safe and optimal continuity of care.
‘The handover process will continue to be error-prone unless systems are put in place to improve communication, minimise risks, and effectively standardise the entire handover process’
Scope of the problem
Bruce and Suserud (2005) raised concerns that ambulance-borne patients transported to hospitals are usually the most seriously afflicted; therefore, the interplay between pre-hospital and hospital personnel is vital in conveying important health information at handover. Although clinical handover information being lost in translation is not unique (Solet et al 2005) to the paramedic-ED staff interface, the process may be affected by cultural issues, lack of multidisciplinary training, and professional recognition of handover importance (Jensen et al, 2013).
The Joint Commission's report (2014) on Sentinel Event Data 2004–2014 identified ineffective communication during handover as one of the most common root causes for these sentinel events. Bost et al (2010) reported that there are knowledge gaps in terms of handover information, consequences of poor handover, transfer of responsibility, staff perception of handovers, staff training and evaluation of recommended strategies to improve clinical handover. In a further study, Bost et al (2012) concluded that handover errors are common between ambulance personnel and the ED, and there is a need for standardisation of handover responsibilities and development of structured handover protocols.
A study of closed malpractice claims in the United States of America found that inadequate handover was a contributing factor leading to missed or delayed diagnosis in an ED in 24% of cases (Kachalia et al, 2007). Similarly, Gandhi et al (2006) reported that 20% of diagnostic errors were attributed to failure in handover during ambulatory care, further highlighting the importance of adequate clinical handover.
All these reports suggest that an ineffective handover in any healthcare setting can have many detrimental effects on the patient's safety and quality of care provided. The handover process will continue to be error-prone unless systems are put in place to improve communication, minimise risks, and effectively standardise the entire handover process.
Standardisation of the handover protocol
Implementing standardised handover protocols has been found to improve the handover process by preventing communication related delays, errors, and omissions in patient care (Redfern et al, 2009; Farhan et al, 2012; Iedema et al, 2012; Meisel et al, 2015).
The Joint Commission Centre for Transforming Healthcare (2014) identified the lack of standardised handover procedure as a validated root cause for failed handover communication. The Accreditation Council for Graduate Medical Education (2015: 19) states: ‘Sponsoring institutions and programmes must ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety.’ The Australian National Safety and Quality Health Service Standards (Australian Commission on Safety and Quality in Healthcare, 2012) also require health service organisations to implement an effective clinical handover through developing and implementing an organisational system for structured clinical handover.
Iedema et al (2012) reported that the standardisation of the paramedic-ED staff communication interface led to improvements in how information was relayed by the paramedic, the amount of information that was relayed, the time it took to relay the information, and the number and type of questions asked about the information handed over.
There are two guiding principles for standardisation of a handover protocol: first, it should be tailored according to the discipline (end users), and second, both the processes and the contents of the handover should be standardised in the order or form it is presented (Arora and Johnson, 2006; Australian Commission on Safety and Quality in Healthcare, 2012).
Standardisation of the processes implies identifying the entire steps in a clinical handover and then improving each of these steps, as well as identifying who should be present during a clinical handover. Standardisation of the contents will help in creating a shared set of expectations between the sender and receiver of the handover, i.e. all participants will be aware of the information (content) that they are required to know, communicate, and act upon. Acronyms and mnemonics can be used to help structure the contents of a clinical handover, as they facilitate rapid information recall, especially when it relates to non-technical skills (Logarajah and Alinier, 2014). We present here two such acronyms, SBAR and IMIST-AMBO, to explore their role in facilitating a complete, concise and structured handover at the paramedic-ED interface, while meeting the informational expectations of the ED staff, for both medical and trauma cases. Although other acronyms exist (Riesenberg et al, 2009; Starmer et al, 2012), they are not discussed in this article.
SBAR (Situation, Background, Assessment, and Recommendation)
SBAR is a framework of communication originally developed by the US Navy and later adopted by other industries, including health care, to structure information when team members communicate with each other (Pope et al, 2008; Marshall et al, 2009; Institute for Healthcare improvement, 2015). It was found to be the most frequently cited handover acronym in one systematic review (Riesenberg et al, 2009). ISBAR is a modification of SBAR, to put more emphasis on identification of the sender, receiver, and patient, so as to promote the introduction of who is performing the handover and communication of the patient's name, gender, and age, and to confirm one is addressing the appropriate recipient or receiver (Marshall et al, 2009; Thompson et al, 2011; Dawson et al, 2013).
In the hospital setting, SBAR provides a model for team members to share patient-specific information in a concise and structured format, and with a shared set of expectations between the sender and the receiver. Although SBAR helps to structure communication, it does not explicitly specify the necessary data set in each of its components that needs to be communicated (Table 1). Paramedics in some contexts have diverse educational and training backgrounds, and generally very limited knowledge of their patients due to the short duration of the encounter, hence the use of SBAR might lead to wide variations in the contents and order of information of the handover provided. The paramedic has to convey multiple sets of information in each of the four components of SBAR in order for the clinical handover to be complete and omission free.
| Components of SBAR | Information expected in the respective components |
|---|---|
| Situation | The sender (paramedic) states who they are, identifies the patient, and then states what has happened for this handover communication to be taking place, i.e. presenting the patient's chief complaints, symptoms, or mechanism of the injury. |
| Background | The sender conveys other information related to the chief complaint, past medical history, medication history, and allergies. |
| Assessment | The sender provides details regarding the Glasgow Coma Scale (GCS), latest vital signs, trends, and physical examination findings, a brief assessment of the overall patient status, the most probable diagnosis, and what action and treatment have been provided so far. |
| Recommendations | The sender finally, based on their interaction with the patient, states their recommendations for immediate actions, mentions if the patient is time critical or not, and makes sure the recipient reads-back and understands what information was conveyed. |
Although the use of the SBAR framework has been recommended to improve handover communication (WHO Collaborating Centre on Patient Safety Solutions, 2007), there are factors such as physical and mental stress from the unique uncontrolled pre-hospital environment, chaotic ED environment, and frequent interruptions which can result in paramedics’ omission or non-conveyance of information within each component of the SBAR tool. ‘Recommendations’ may or may not be made by paramedics and may be influenced by ED environmental reception factors and professional hierarchy. Omission of contents that may appear insignificant can be a major cause of failed communication during handoffs (Arora et al, 2005).
In a randomised trial using a simulated on-call setting whereby telephone communications were taking place between nurses and physicians, Joffe et al (2013) found that using the SBAR framework did not improve communication content or time. The background cues were communicated less often when SBAR was used, potentially highlighting a training issue with the use of SBAR by the study population, who may have attempted to over-filter the information to be verbalised. This study is relevant because paramedics often use wireless technology to provide pre-arrival information to the ED staff in an abridged form.
Loseby et al (2013) argue that the SBAR does not prompt paramedics to convey key points in a trauma patient such as mechanism of injury, the injuries sustained, and the clinical interventions performed. There is, however, support for the adoption and further evaluation of a trauma handover template, since it can provide valuable structure to the face-to-face handover and reduce information loss (Evans et al, 2010).
IMIST AMBO
The ‘IMIST-AMBO’ acronym (Table 2) was originally designed by Jacinta Young, an Australian intensive care paramedic, to help colleagues convey patient-related information during a clinical handover in a precise manner and a specific order (Iedema and Ball, 2010).
| I | Identification (patient)* |
| M | Mechanism of injury/medical complaint |
| I | Injuries/information related to the complaint |
| S | Signs and symptoms including GCS and vital signs |
| T | Treatment given and trends noted |
| A | Allergies |
| M | Medications (patient's regular medications) |
| B | Background history (patient's past history) |
| O | Other information (scene, social, valuables, advanced directives, family informed) |
The IMIST-AMBO tool guides the paramedic not only to structure the communication but also to remember the necessary data set that need to be conveyed during an urgent or emergent clinical handover. Iedema et al (2012) found an improvement in handover communication between ambulance paramedics and ED clinicians following the introduction of the IMIST-AMBO acronym. When IMIST-AMBO was used, there was a consistent ordering of the information, greater frequency of the necessary data set being conveyed and a reduction in information repetition. Overall it met the informational expectations of ED clinicians. A second analysis of the implementation of the IMIST-AMBO protocol revealed that the amount of information given by paramedics had increased, while the duration of handovers had been reduced from 96 to 83 seconds (Dean, 2012).
However, further research is needed to understand its acceptance by paramedics across different global health systems and to identify training requirements necessary to ensure correct implementation of this tool.
Discussion: which handover acronym (SBAR vs. IMIST-AMBO) best suits the paramedic-ED interface?
There is no single handover tool that is ideal for all handover situations. A handover tool that works in one discipline or context may not work in another, because every discipline has unique requirements when it comes to the contents of a clinical handover (Arora and Johnson, 2006; Australian Commission on Safety and Quality in Healthcare, 2012). Paramedics have to adopt a handover tool which is easy to remember, concise, complete, tailored to paramedic-ED handover, and which should also align with the informational expectations of the ED staff, for medical as well as trauma patients.
Each letter in the IMIST-AMBO tool prompts the paramedic to provide ED staff a specific set of information about a clinical case that is essential to convey (Table 2), while not clouding the clinical handover with other unnecessary information. Furthermore, IMIST-AMBO has been specifically designed for the paramedic to ED staff clinical handover interface. It is currently being rolled out for use by Hamad Medical Corporation Ambulance Service paramedics with all ED departments across Qatar. The template used can be seen in Appendix 1.
One concern is that IMIST-AMBO might not align with the expectation of the ED staff, since SBAR is frequently used as a communication framework among doctors and nurses within the hospital setting (Riesenberg et al, 2009; Loseby et al, 2013). A closer look at both tools side-by-side clearly shows that IMIST-AMBO is essentially a breakdown of the four components of SBAR, although in a slightly different sequence (Figure 1).
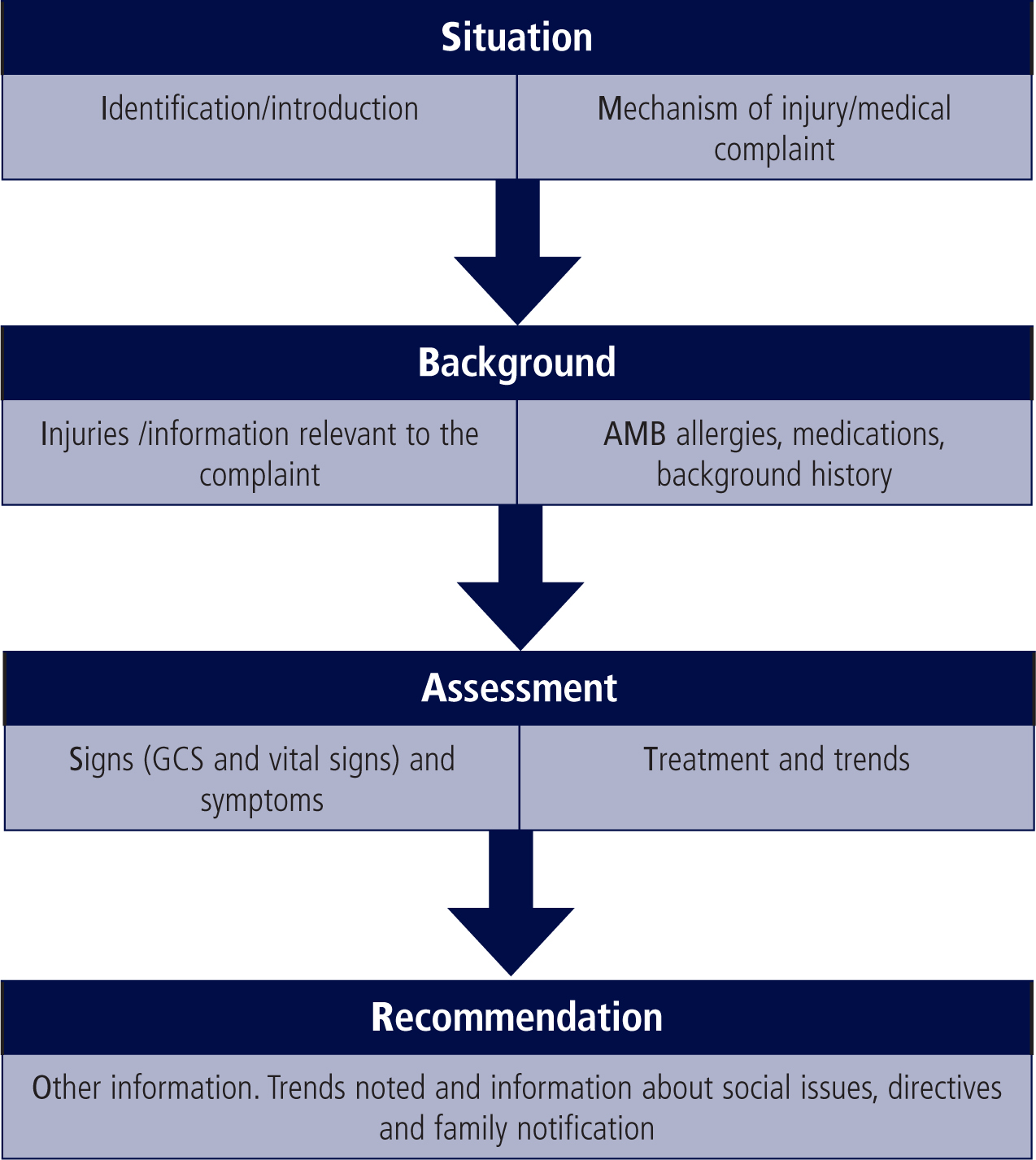
Three considerations from Figure 1 are noteworthy:
Limitations
This review article focuses on the use of SBAR and IMIST-AMBO for structuring the content of clinical handover between paramedics and ED staff. It does not provide details on other aspects of clinical handover, such as training for implementation; and human factors aspects, such as attentiveness, mutual respect, adherence to protocols, and cultural and language differences among people involved in handover. All of these constitute the potential barriers to an effective handover and are presented in more detail in Table 3.
|
|
It is important to note that each ambulance service/ED globally, will have their own set of root causes for ineffective clinical handover (sometimes beyond those presented in Table 3), the identification of which is the key to devising targeted solutions to improve patient safety (Joint Commission Centre for Transforming Healthcare, 2014).
Conclusions
Paramedics have to adopt a handover tool which is concise yet provides all key clinical information, tailored to the paramedic-ED handover interface, and which also aligns with the informational expectations of the emergency department staff, for medical as well as trauma patients.
Gathering information during the short duration of care in an uncontrolled pre-hospital environment may be challenging for paramedics. The IMIST-AMBO tool which is specifically designed for the paramedic-ED handover interface prompts the transfer of key clinical information that is explicitly structured and well-ordered in terms of criticality to cater for routine pre-hospital care, without clouding the clinical handover with other unnecessary information for the ED clinician. The SBAR tool, in contrast, is a situational briefing model adapted from the military. It does not explicitly prompt for some of the patient related information, which may lead to omission or non-conveyance of key elements during paramedic-ED staff handover.
Furthermore, IMIST-AMBO also aligns itself with the SBAR communication framework commonly used within the hospital setting. This, however, requires both paramedic and ED staff to understand the similarities and cross matching between both tools, which can be achieved by joint training on the subject. The limited number of quantitative and qualitative studies looking at the use of IMIST-AMBO mandates further work to understand its acceptability and acceptance by paramedics across different global health systems and to identify training requirements necessary to ensure correct implementation of this tool.
‘Paramedics have to adopt a handover tool which is concise yet provides all key clinical information, tailored to the paramedic-ED handover interface’
